Modifier 24 - Guide on when, how, and what to use it for
Modifier 24 Quick Summary
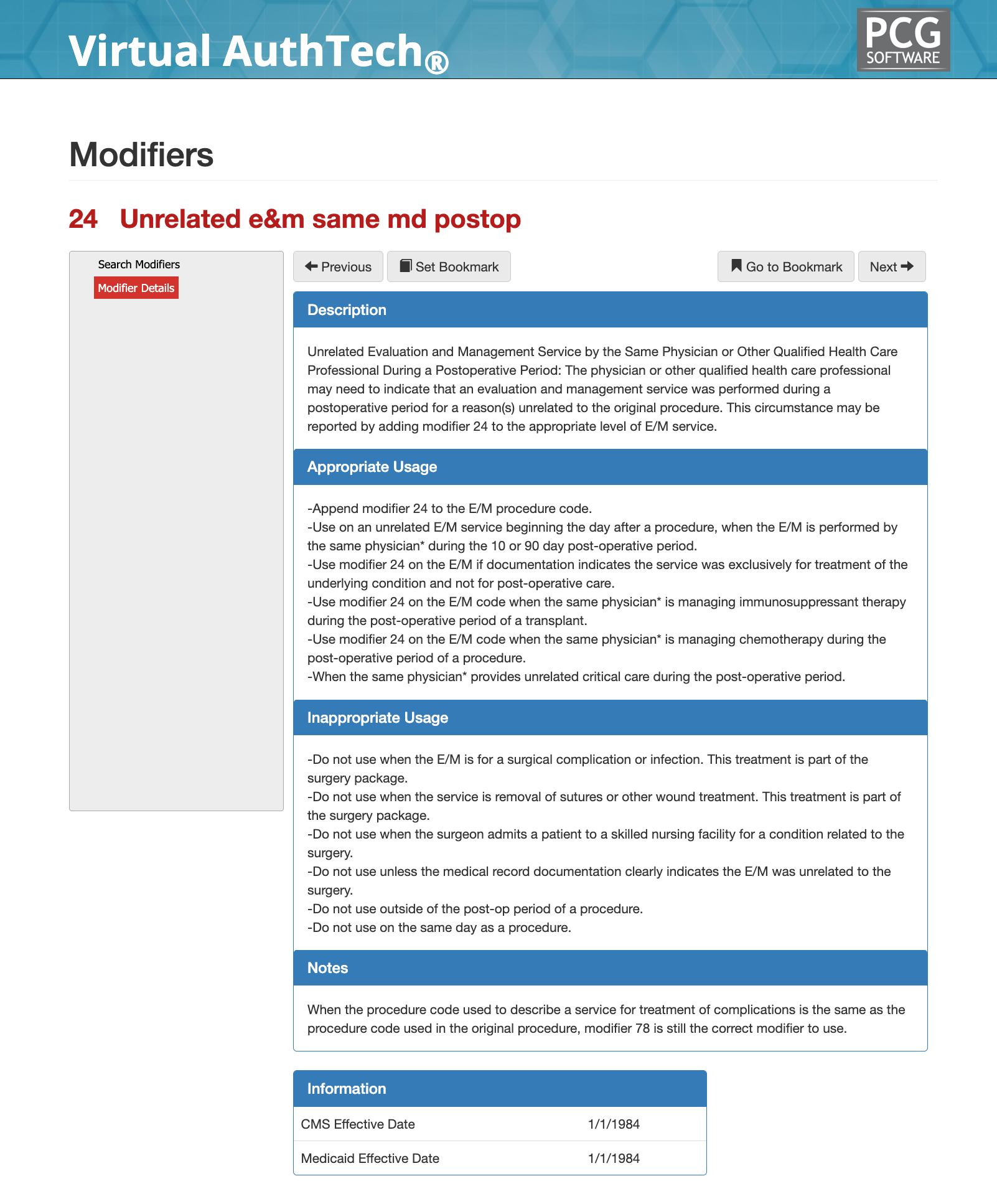
Modifier 24 is used to report an evaluation and management (E/M) service that is unrelated to the original surgical procedure and performed by the same physician or qualified health care professional during the postoperative global period. Its purpose is to distinguish medically necessary E/M services for new or separate conditions from routine postoperative care that is already included in the global surgical package.
From a payer and audit perspective, Modifier 24 does not override the global period itself. Instead, it signals that the E/M visit is clinically independent of the surgery and therefore eligible for separate reimbursement when supported by appropriate documentation.
Modifier 24 Description & Usage
Modifier 24 indicates that an E/M service performed during a postoperative period is unrelated to the surgical procedure that initiated the global period. It applies only to E/M services and may be appended to office, outpatient, inpatient, or critical care E/M codes when the visit addresses a separate diagnosis, complaint, or clinical condition.
The modifier may be used only when the E/M service begins after the day of surgery and is performed by the same physician or qualified health care professional who performed the original procedure. Services rendered on the same day as surgery generally fall under Modifier 25, not Modifier 24.
When can I use Modifier 24 appropriately?
Modifier 79 should be used when all of the following conditions are met:
- A procedure is performed during the postoperative (global) period of a prior procedure
- The new procedure is unrelated to the original surgery
- The service is performed by the same physician or qualified health care professional
- The service is not staged, planned, or related to the original procedure
- The service begins after the day of surgery (not on the same day)
Typical scenarios include treatment of a new condition, injury, or diagnosis that arises independently during the global period of a previous procedure. From a claims adjudication standpoint, Modifier 79 tells the payer that the global surgical package does not apply to the subsequent service and that a new global period may begin based on the second procedure’s global assignment.
Example: New Medical Condition During Global Period
A patient undergoes total knee arthroplasty and later presents during the global period with acute shortness of breath and chest pain. The surgeon performs an E/M visit that results in evaluation and referral for suspected pulmonary embolism. Documentation clearly establishes a new medical problem unrelated to orthopedic postoperative care, supporting appropriate use of Modifier 24.
When is it not appropriate to use Modifier 24?
Modifier 24 should not be reported when the E/M service is related to the surgical procedure or postoperative recovery. This includes evaluation of surgical pain, wound checks, suture removal, infection management, expected complications, or routine postoperative visits. It should also not be used for services performed on the same day as surgery, for staged or planned postoperative care, or when the documentation does not clearly differentiate the visit from postoperative management.
Example: Postoperative Wound Evaluation
A patient returns two weeks after abdominal surgery with redness and drainage at the incision site. The surgeon evaluates the wound, prescribes antibiotics, and documents postoperative infection management. This E/M service is part of postoperative care and should not be reported with Modifier 24.
Modifier 24 and Global Surgical Periods
Modifier 24 does not reset or override the global surgical period. Instead, it allows separate reimbursement for an E/M service that is unrelated to the procedure responsible for the global period. Payers rely heavily on the Medicare Physician Fee Schedule global indicators when adjudicating Modifier 24 claims. While the modifier may be reported during 10- or 90-day global periods, approval depends on clear evidence that the visit is clinically independent and not a continuation of surgical care.
Example: Chronic Disease Management During Recovery
A patient recovering from hernia repair presents for management of uncontrolled diabetes during the postoperative period. The E/M visit focuses exclusively on medication adjustments and laboratory review related to diabetes, with no reference to surgical recovery. This supports appropriate use of Modifier 24.
Documentation Requirements for Modifier 24
Strong documentation is essential for Modifier 24 compliance. The medical record should clearly establish a separate chief complaint, an independent diagnosis, and clinical decision-making unrelated to the surgery. Operative recovery should not be the focus of the note, and postoperative language should be avoided unless explicitly excluded as the reason for the visit.
Documentation that merely states “unrelated to surgery” without clinical explanation is insufficient and commonly flagged during audits.
Example: Clear Clinical Separation in Documentation
A patient seen during a postoperative period for evaluation of newly diagnosed atrial fibrillation has a note that includes a distinct history, cardiac exam findings, ECG interpretation, and treatment plan unrelated to the surgical site. The note does not reference surgical healing or recovery, supporting compliant Modifier 24 reporting.
Helpful tips on Modifier 24
Modifier 24 vs Modifier 25 vs Modifier 79
Modifier 24 applies only to E/M services during a postoperative period that are unrelated to surgery. Modifier 25 applies to same-day E/M services that are significant and separately identifiable from a procedure. Modifier 79 applies to unrelated procedures, not E/M services, performed during a global period. Incorrect substitution among these modifiers is a common cause of denials, recoupments, and audit findings.
Common Modifier 24 Denials Triggers and Payer Logic
Modifier 24 claims are frequently denied when diagnosis codes overlap with the original surgical condition, when documentation resembles routine postoperative care, or when visit timing suggests expected follow-up. Repeated use of Modifier 24 by the same provider during global periods may also trigger audits. From a payer adjudication perspective, Modifier 24 does not guarantee payment. Claims systems and reviewers analyze diagnosis relationships, documentation language, and historical claim patterns to determine whether the E/M service truly stands apart from postoperative care.
Compliance Considerations for Modifier 24
Modifier 24 is considered a high-risk modifier from a compliance standpoint because it directly affects global surgical reimbursement. Overuse or inappropriate application may be interpreted as an attempt to unbundle postoperative care. Best practices include reserving Modifier 24 for clearly unrelated conditions, ensuring documentation reflects distinct clinical reasoning, and avoiding its use when postoperative care could reasonably be expected. Health plans and auditors often view improper Modifier 24 usage as a signal for broader coding pattern review.
Summary on Modifier 24
Modifier 24 allows appropriate reimbursement for medically necessary E/M services that are unrelated to a surgical procedure and performed during the postoperative global period. When used correctly, it supports accurate claims processing and fair payment. When misused, it is among the most frequently scrutinized modifiers by payers and auditors. Clear documentation, distinct diagnoses, and disciplined application are essential to compliant Modifier 24 reporting and long-term revenue protection.
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others