✅ Higher First-Pass Approval Rates
✅ Fewer Denials and Appeals
✅ Reimbursement Contract Tool
✅ HIPAA Compliant
iVECoder® for Medical Billers
Best Coding Validation Software for Billing Companies
Every Denial Reduces Profitability
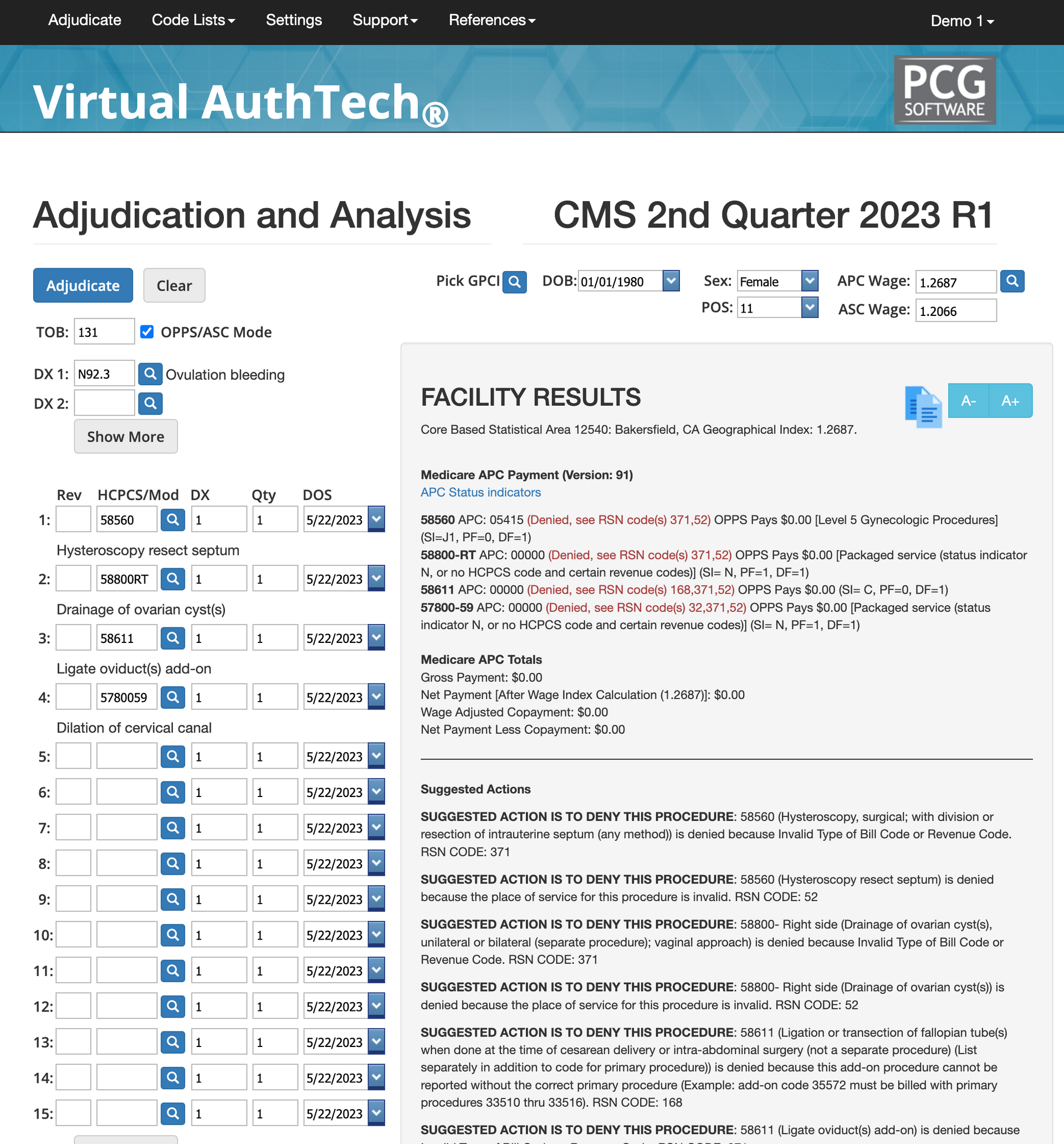
Every denied claim slows reimbursements, adds rework, frustrates providers, and shrinks margins for both your billing company and your clients. These denials rarely happen because your team made a mistake—most occur because CPT®, CMS, AMA, Medicaid, and commercial policies all update at different times while coding books only update once a year. iVECoder® gives billing companies the advantage they’ve been missing:
quarterly rule updates and AI-powered mock adjudications that reveal every reason a claim could be denied before it ever reaches the payer. Your team submits cleaner claims, reduces appeals, and helps clients get paid faster with fewer surprises.
Preventing Provider Denials
Target your most commonly denied codes
Run a 6-month denial report to identify the codes your billing team struggles with most. Then use iVECoder for 30 days to retrain how those claims should be submitted. Repeat the cycle until first-pass approvals rise—and continue refining until your clients consistently achieve 97–99% first-pass rates.
Identify the Reasons for Denials
Denials rarely occur because a biller or coder “made a mistake.” They happen because CMS, AMA, Medicaid, and commercial payer rules change constantly—while most coding books and scrubbers update only once a year. Add in conflicting guidance, missing or incorrect modifiers, terminated codes, global period quirks, and payer-specific rules, and it becomes nearly impossible for billing companies to stay fully compliant without software that keeps pace.
How iVECoder prevents denials
iVECoder analyzes every line of a claim using the exact same adjudication logic payers use. Instead of flagging one issue at a time, it shows every reason a claim might deny—up front. Your team fixes all errors in a single pass, improving first-pass approvals, reducing rework, and helping your clients get paid faster with fewer surprises.
Quarterly Updates Beat Outdated Coding Books
Most scrubbers and references update annually, leaving your billers months behind changing rules. iVECoder updates every quarter using CMS, AMA, Medicaid, NCCI, and state Medicaid policies—ensuring your coding logic always reflects the newest rules and edits. With more than 72 million edits maintained continuously, your team never submits claims using stale or expired guidelines.
What are National Standard statistics?
- 90% minimum 1st pass approval
- Goal of 98% or higher
- $44 per appeal (administrative fee alone)
- CMS issues quarterly changes you're unaware of
- 60% of denials are knowledge gaps
- Coding related errors are avoidable with iVECoder
AI Medical Coding Database
Research codes, learn, and reduce denials
Unlike coding books and most scrubbers that update only once a year, iVECoder® refreshes every quarter with the latest CMS, AMA, Medicaid, and CCI guidelines. Your coding team always works from the most accurate, most compliant rule set—no outdated edits, no guesswork, no surprises.
iVECoder® allows you to quickly search:
✅ CPT
✅ HCPCS
✅ ICD-10
✅ APC
✅ ASC
✅ GPCI
✅ NDC
✅ Crosswalks
✅ Modifiers
✅ Bundled Codes
✅ Related Codes
✅ Primary Codes, and more.
Bundled codes create non-compliance
undled codes are one of the biggest—and most preventable—sources of denials for billing companies. iVECoder shows your team exactly which CPT, HCPCS, and APC codes are bundled together, under what conditions, and whether a service is separately billable, included in a global period, or restricted by CCI edits. Instead of sorting through outdated manuals and payer PDFs, your billers instantly see compliant combinations before claims ever reach the payer. This reduces write-offs, prevents downstream appeals, and keeps your provider clients profitable and compliant.
Research codes to improve clinical documentation
Unclear or incomplete provider documentation is one of the most common causes of denials. iVECoder allows your billing teams to review official descriptions, modifiers, clinical requirements, and payer rules behind each code—so they can identify exactly what must be documented before submitting a claim. By aligning documentation with coding rules, your clients experience fewer medical-necessity denials, fewer documentation requests, and stronger approval rates on both initial submissions and appeals.
Using iVECoder for new and existing client audits
iVECoder doubles as an audit-prevention system. Your team can search CPT, HCPCS, ICD-10, modifiers, bundled codes, crosswalks, and related code families to uncover billing patterns that typically trigger payer audits. The system highlights frequency issues, coverage limitations, improper code combinations, outdated rules, and high-risk edits—giving your billing staff the ability to correct claims before submission. This helps your company stay audit-ready, protect your provider clients, and reduce risk long before payers flag a problem.
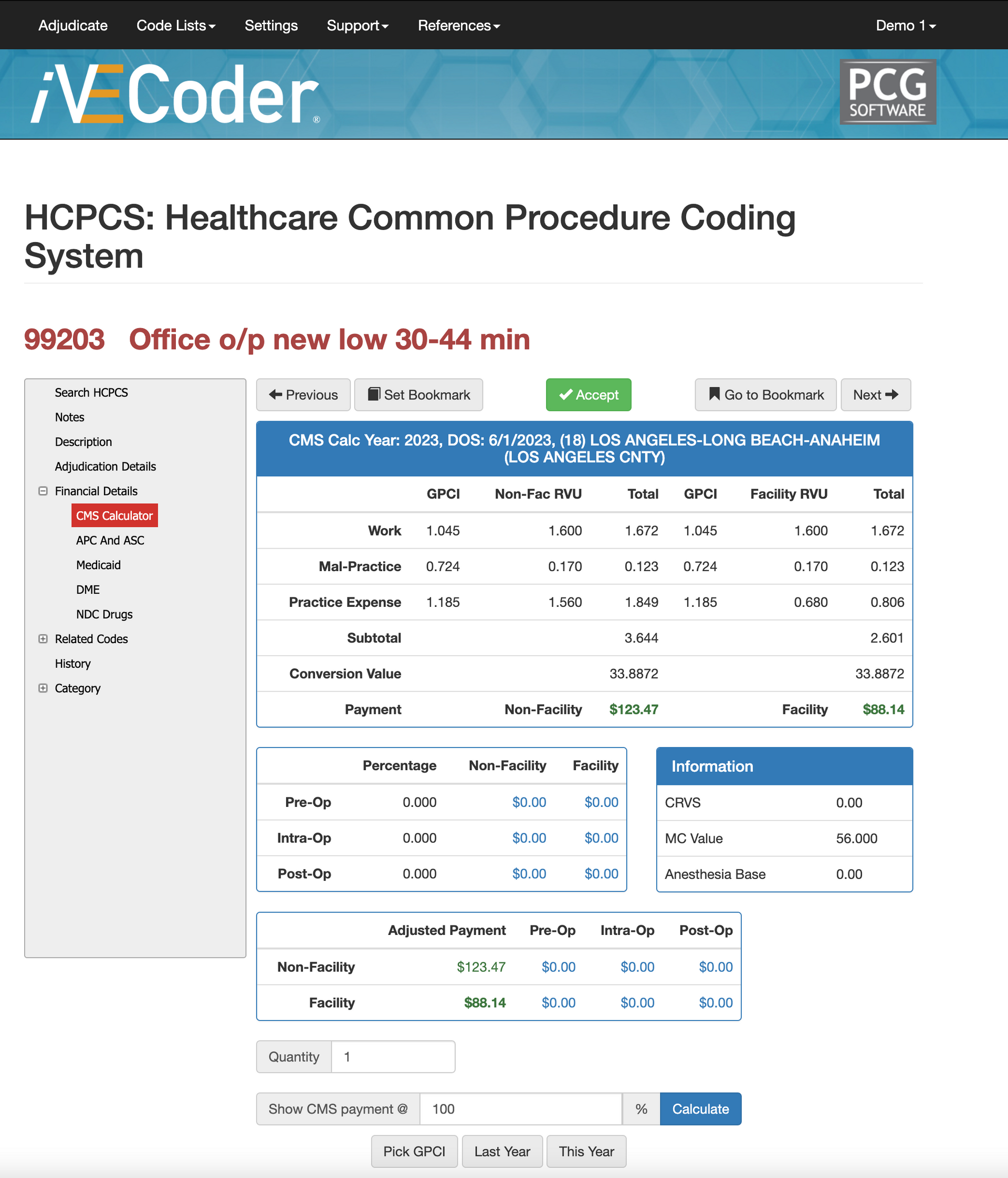
Help Providers Improve RVU Rates
Negotiate per Code not Across the Board...
Most providers accept broad, across-the-board rate changes—often without realizing which individual codes are undervalued or underpaid. iVECoder® gives billing companies the data needed to renegotiate at the code level, using RVUs, GPCI values, and CMS benchmarks to prove the true value of your clients’ clinical work. This helps your billing company advocate for fair, market-aligned reimbursements—even for complex or high-efficiency procedures.
Identify Underpaid Rates
iVECoder® instantly flags CPT and HCPCS codes where contracted payer rates fall far below CMS or GPCI-adjusted benchmarks. Your billing team can pinpoint underpaid, high-volume codes and bring hard data into negotiations. Instead of asking for blanket increases, you renegotiate specific codes with evidence—closing reimbursement gaps and increasing overall revenue.
Compare Facility vs Professional Rate
Reimbursement can vary dramatically between facility and non-facility settings. iVECoder® breaks down RVU values for each environment so you can identify discrepancies between what CMS pays and what your contracted rates reflect. This helps you push back when payer schedules misalign with CMS totals, prevent silent underpayments, and ensure your clients get paid the true value of their services.
Analyze Payer Variance and Gaps
Two payers can reimburse the same code at wildly different rates. iVECoder® compares fee schedules side-by-side to expose outdated contracts, inconsistent rate structures, or large underpayment gaps. This shows your billing team exactly which contracts should be renegotiated first—and which codes provide the highest revenue lift for your providers.
What does iVECoder Cost?
Below you will find our three iVECoder pricing plans we can discuss during your FREE demo and FREE trial. Please be aware that iVECoder can only be used by individuals within the United States and US territories at this time. This is not our requirement; it is the AMA licensing requirement we have to abide by.
$99 per User
Month to Month Terms
Perfect for billing teams that need agility without long-term commitments. Month-to-month access gives your coders and billers real-time rule validation, cleaner claim submissions, and stronger documentation for every provider you support. With quarterly CMS/AMA/Medicaid updates included, your team always codes using the most current rules—no outdated books, no guesswork, and no disruption when payer rules shift.
$999 per User
Great Discount for Annual Terms
Our most popular option for billing organizations focused on accuracy, consistency, and predictable costs. Annual users receive the full rule engine, bundled-code validation, mock adjudication tools, and quarterly updates—paid once for the entire year. This plan gives billing companies reliable budgeting, improved coding confidence, and guaranteed savings over month-to-month access.
$1,999 per User
Huge Discount for 3 Year Term
Designed for billing companies that want long-term pricing stability and uninterrupted access. This discounted three-year license locks in the lowest per-user cost while delivering continuous rule updates, CMS/AMA/Medicaid quarterly changes, and unlimited mock adjudications. Your team never has to worry about expirations, renewals, or monthly billing—just consistent accuracy, compliance, and long-term operational savings.
Get a FREE Trial and Demo
In 20 minutes you'll see the coding magic!
Describe that they come to the meeting with a list of possible codes important to them, our CSO will show you how fast and accurate it is, how to use to negotiate new RVU rates, and more, then we give you a free 14-day trial.
Contact Us
We will get back to you as soon as possible.
Please try again later.



