✅ Less Denials
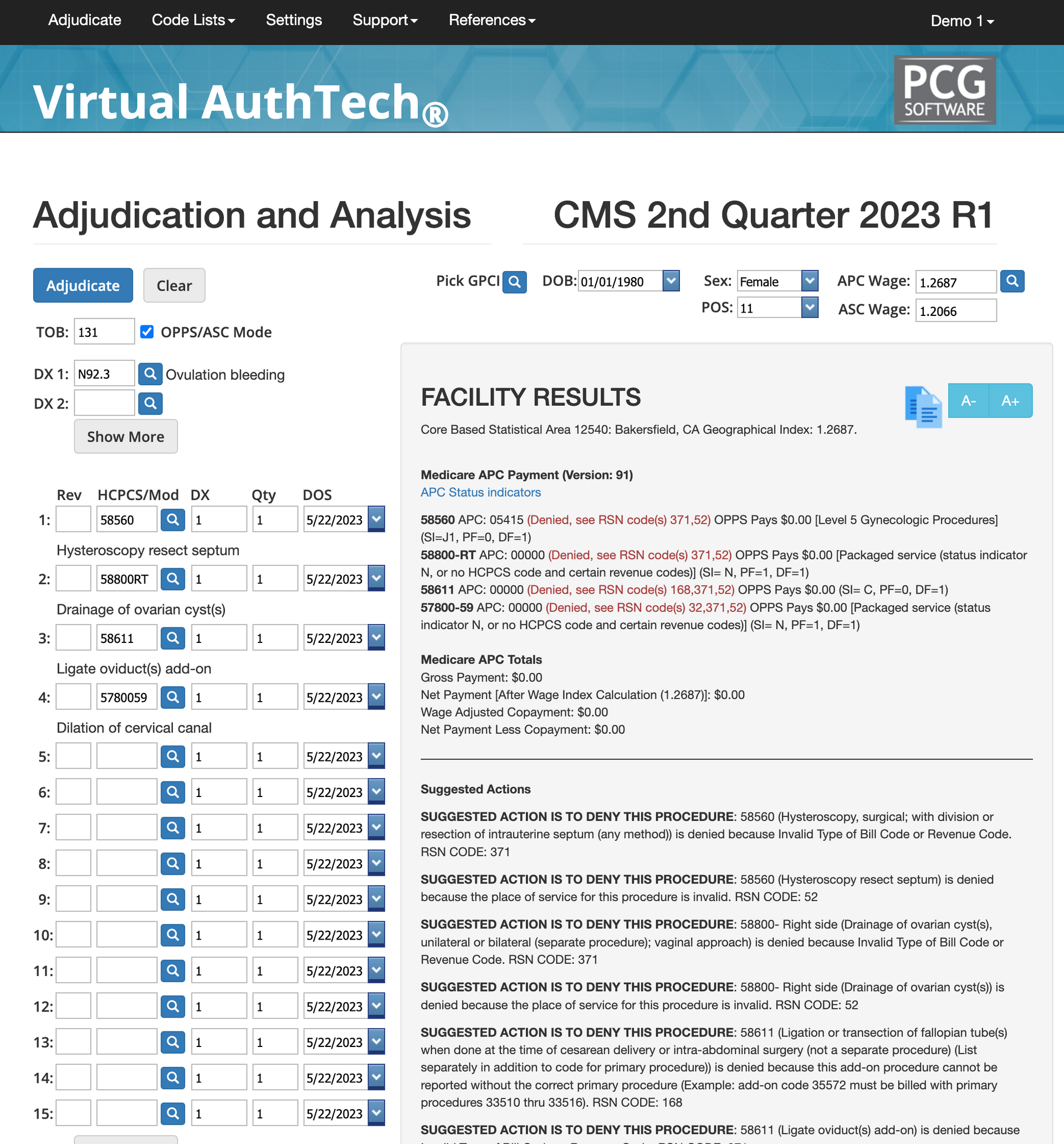
✅ Run Mock Claims and Auths
✅ Reimbursement Contract Tool
✅ HIPAA Compliant
✅ Month-to-Month Terms
iVECoder® for Providers
Best Code Scrubber for Providers and Clinics
Denials are costly but not your fault!
Every denied claim costs time, revenue, and an average of $44 per appeal -and most denials happen simply because the rules are impossible to keep up with. CPT®, CMS, AMA, and Medicaid guidelines change constantly, payer policies differ, and coding books update only once a year. Your team isn’t the problem. Outdated tools are.
iVECoder® fixes this by giving billers, coders, and providers the most up-to-date rules
every quarter, plus AI-powered mock adjudications that show every reason a payer could deny your claim—before you submit it.
Reduce Denials in 30 days
Target your most commonly denied codes
Run a 6-month denial report to identify your most commonly denied codes, then use iVECoder for 30 days to learn how to submit these claims correctly. Then repeat the process until your first pass approval rate grows, then rinse and repeat until your claims submission has 97-99% first pass approval rates.
Why denials happen in the first place?
Denials rarely occur because a coder "made a mistake." They happen because CMS, AMA, Medicaid, and commercial payer rules change constantly—and each payer interprets those rules differently. By the time coding books and most scrubbers update (once a year), the rules are already outdated. Add in conflicting diagnoses, incorrect modifiers, terminated codes, global periods, and payer-specific quirks, and it’s nearly impossible to stay compliant without software that evolves with the rules. iVECoder gives you real-time clarity into why denials happen so you can stop them before they occur.
How iVECoder prevents denials before submission
iVECoder analyzes every line of a claim using the same criteria payers use to deny, pend, or reduce payment. Instead of showing one error at a time—like most scrubbers—it instantly shows every reason a payer might reject the claim. This gives your billing team the power to fix all issues in one pass, improving first-pass approval rates and helping your team submit fully compliant claims the first time. No guesswork, no blind submissions, and no more denial ping-pong.
Quarterly updates vs Outdating CPT books
Most coding resources update once a year, leaving billers working with outdated information for months at a time. iVECoder updates every quarter using the latest CMS, AMA, Medicaid, NCCI, and state Medicaid updates—ensuring your coding logic always matches current rules and edits. With 72+ million edits and continuous maintenance, you’re never working from stale or expired guidelines again. Staying compliant becomes automatic.
AI Medical Coding Database
Research codes, learn, and reduce denials
Unlike coding books and most scrubbers that update only once a year, iVECoder® refreshes every quarter with the latest CMS, AMA, Medicaid, and CCI guidelines. Your coding team always works from the most accurate, most compliant rule set—no outdated edits, no guesswork, no surprises.
iVECoder® allows you to quickly search:
✅ CPT
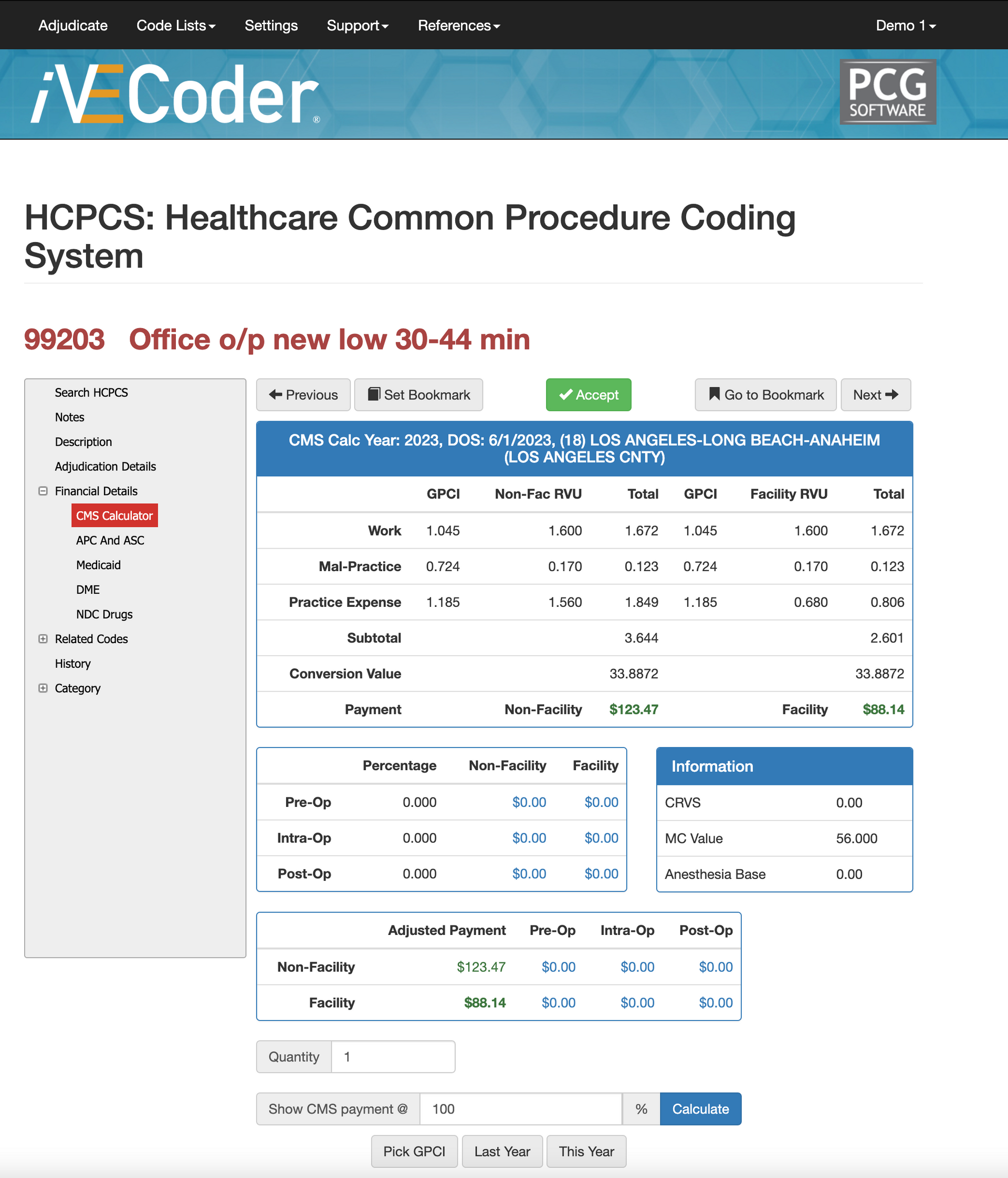
✅ HCPCS
✅ ICD-10
✅ APC
✅ ASC
✅ GPCI
✅ NDC
✅ Crosswalks
✅ Modifiers
✅ Bundled Codes
✅ Related Codes
✅ Primary Codes, and more.
Researching bundled codes
Bundled codes are one of the top reasons claims get denied, reduced, or partially paid. iVECoder makes it simple by showing you exactly which CPT, HCPCS, and APC codes are bundled together—and under what conditions. Instead of searching through outdated PDFs or payer manuals, you can instantly verify whether a service is separately billable, included in a global period, or restricted by CCI edits. This helps your team avoid unbillable combinations, submit compliant claims, and prevent denials before they ever reach the payer.
Research code descriptions to improve clinical notes
Unclear, missing, or incomplete clinical notes are one of the most common causes of medical necessity denials. With iVECoder, you can quickly review official code descriptions, guidelines, and payer requirements to ensure your documentation supports the codes you’re billing. Billers and providers can validate whether the diagnosis aligns with the procedure, whether modifiers are required, and what clinical details must be present. This leads to cleaner notes, fewer documentation requests, and higher approval rates on both claims and authorizations.
How to use iVECoder to find audits?
iVECoder isn’t just a coding tool—it’s an audit discovery engine. You can search by CPT, HCPCS, ICD-10, modifiers, bundled codes, crosswalks, or related code families to identify where billing patterns may trigger payer audits. The system highlights conflicting codes, frequency limitations, improper code combinations, and other red flags that auditors look for. This helps your organization stay ahead of compliance issues, correct problem areas proactively, and reduce risk before payers flag them.
Renegotiate Contracted Rates
Negotiate per Code not Across the Board...
Most providers unknowingly accept across-the-board rate increases or decreases—but that approach rarely reflects the true value of your work. With iVECoder®, you can identify your highest-volume and highest-value CPT and HCPCS codes, spot where your current contracted rates are being underpaid, and use our reimbursement calculator to renegotiate smarter. Instead of blanket adjustments, you renegotiate per code, backed by RVUs, GPCI values, and CMS benchmarks.
This gives your team the data they need to confidently advocate for fair, market-aligned rates—especially for procedures you perform most often or deliver with higher-than-average efficiency.
Identifying Underpaid Codes to Negotiate
iVECoder® makes it easy to identify codes you’re being underpaid for by comparing your contracted rates against CMS, GPCI-adjusted rates, and non-facility/facility benchmarks. This helps you target specific codes where payers are far below the market—your biggest leverage during negotiations. Instead of renegotiating blindly, you renegotiate with proof.
Look at Facility vs. Professional RVU Rates
Use iVECoder® to compare the RVU breakdown for both facility and non-facility settings. Many providers don’t realize how sharply reimbursement changes depending on the place of service. With iVECoder®, you can instantly see whether your contracted rates match real CMS RVU totals—and push back when they don’t. This helps you negotiate with precision, avoid underpayment, and ensure your contracts reflect the true value of your clinical work.
Analyze Payer Variability Across Contracts
Payer reimbursements for the same CPT code can vary dramatically. iVECoder® helps you compare payer fee schedules side-by-side to expose rate inconsistencies, outdated contracts, or large reimbursement gaps. These insights make it easier to prioritize which contracts need renegotiation first—and which codes provide the highest revenue lift.
What does iVECoder Cost?
$99 per User
Month to Month Terms
Perfect for teams who want flexibility without long commitments. iVECoder gives your staff instant access to real-time code validation, cleaner claims, and stronger documentation. With every CMS, AMA, Medicaid, and CCI update included, your team always codes using the most current rules—no outdated books, no guesswork.
$999 per User
Great Discount for Annual Terms
Our best value for organizations committed to accuracy and revenue integrity. Annual users get the same powerful rule engine, mock adjudication tools, and quarterly updates—with guaranteed long-term savings on licensing. A full year of coding confidence, paid once.
$1,999 per User
Huge Discount for 3 Year Term
Lock in three full years of iVECoder access for a single discounted payment. This option gives your team uninterrupted coding accuracy, quarterly CMS/AMA/Medicaid updates, and unlimited mock adjudications without worrying about renewals or monthly billing. It’s the best value for organizations that want long-term stability, guaranteed compliance, and the lowest total cost per user.
Get a FREE iVECoder Trial
In 20 minutes you'll see the coding magic!
Describe that they come to the meeting with a list of possible codes important to them, our CSO will show you how fast and accurate it is, how to use to negotiate new RVU rates, and more, then we give you a free 14-day trial.
Contact Us
We will get back to you as soon as possible.
Please try again later.



