CPT 99203 - Initial Patient Outpaient Consult 30-44 minutes
The full 99203 Billing and Payment Guide
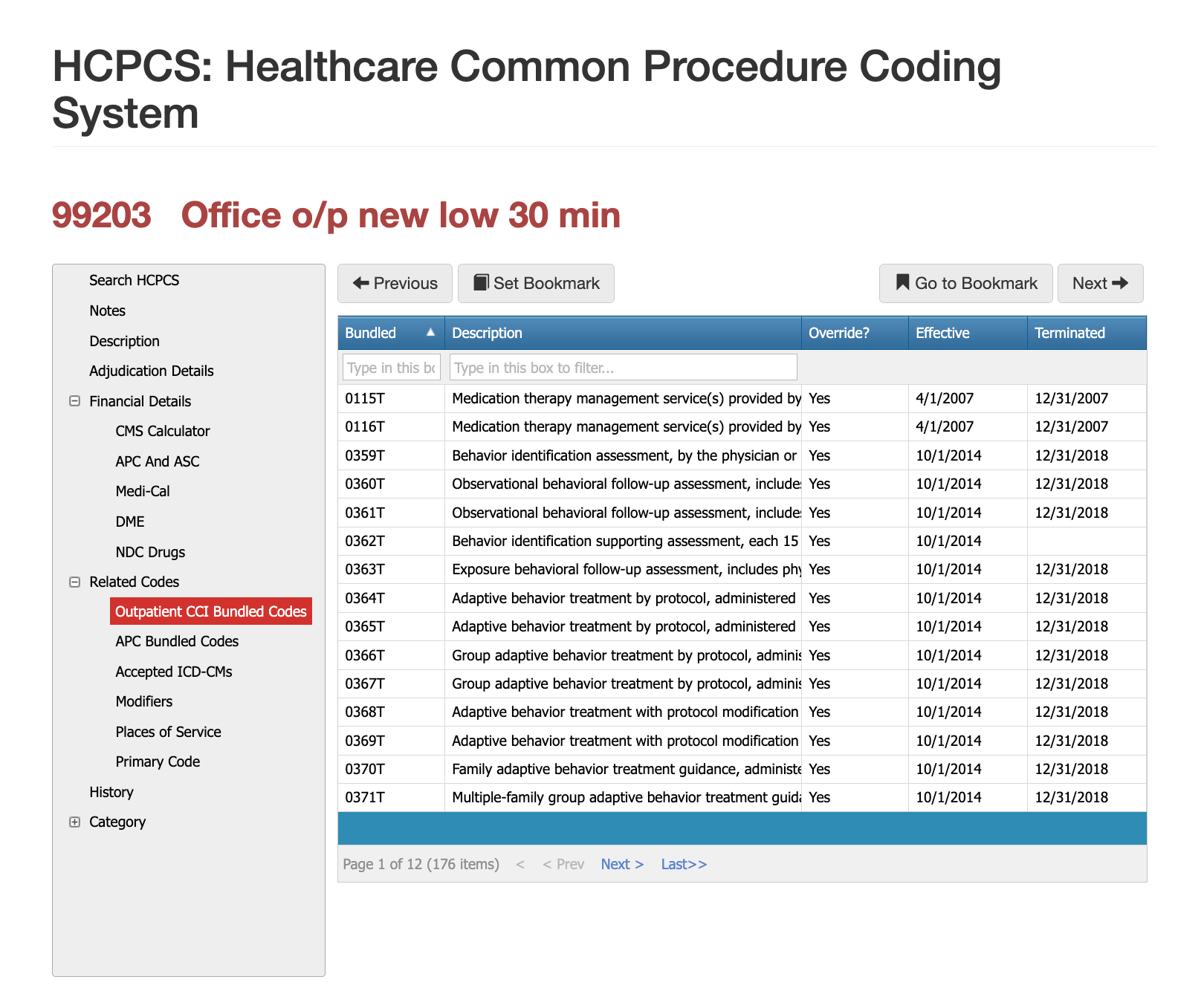
CPT 99203 represents a Level 3 new patient office or outpatient visit, requiring a medically necessary encounter with moderate complexity in history and/or examination and straightforward or low medical decision-making, depending on the documentation year being used. Under the updated CMS E/M guidelines, medical decision-making or total time (30–44 minutes) determines code selection. This code is frequently used in primary care, internal medicine, orthopedics, dermatology, and specialty clinics for new patient evaluations that require more detail than a brief visit but do not rise to high complexity. Because 99203 is a pivotal code in outpatient revenue cycles, payers often review documentation carefully, and compliance teams must ensure accurate MDM, time, and medical necessity alignment.
The Who, What, When for billing and paying for CPT Code 99203
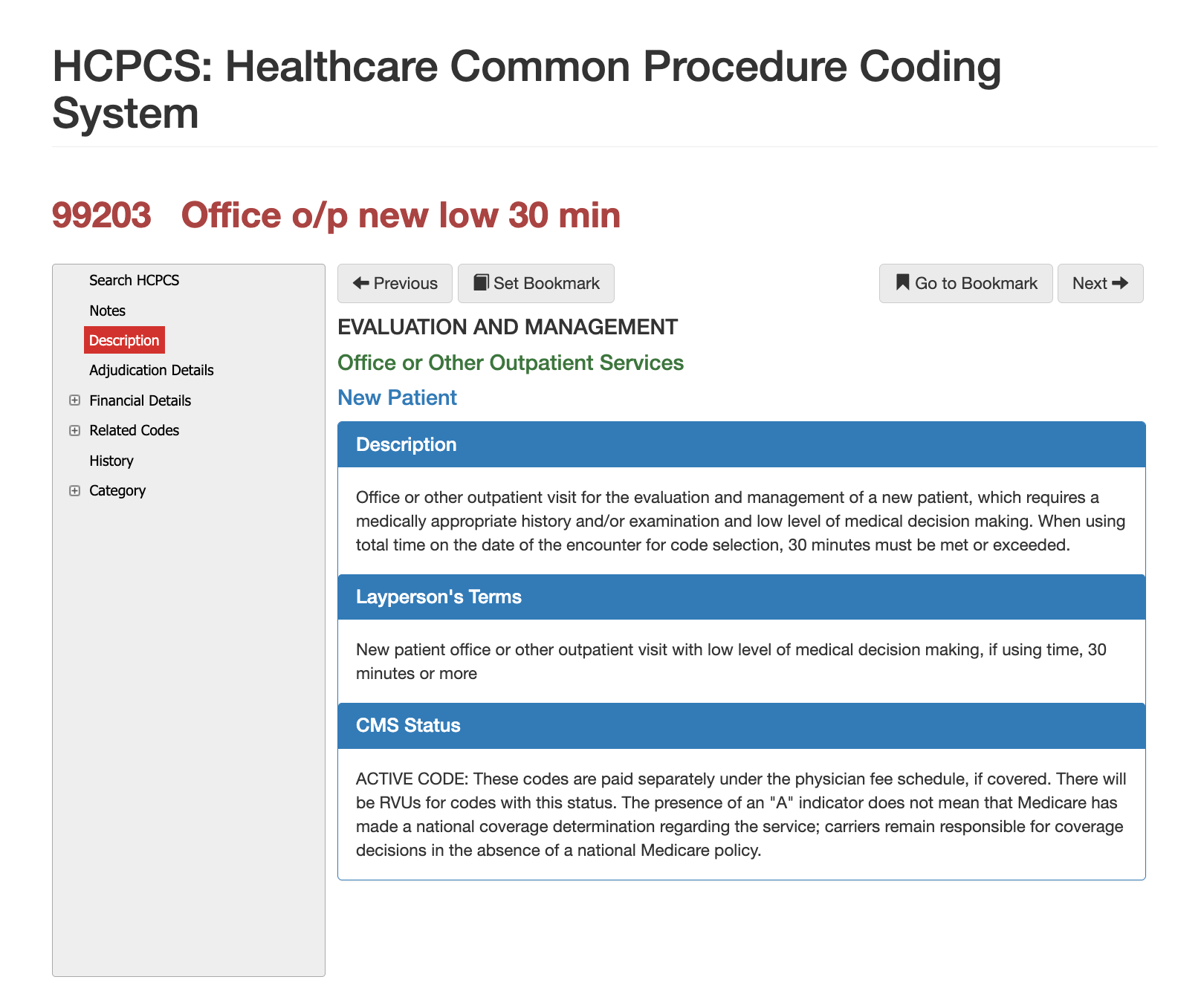
Definition of CPT Code 99203 - AMA vs Layperson:
The AMA defines 99203 as an office or outpatient visit for a new patient that requires a medically appropriate history and/or examination and low-level medical decision-making. Alternatively, the visit may be selected based on total time spent, which must fall between 30 and 44 minutes on the date of service. In simpler terms, 99203 describes an appointment for a patient who has never been seen in the practice before and whose medical situation requires more than a basic evaluation but does not involve extensive testing or high-risk decision-making. The provider must capture enough detail to justify the time and complexity of the visit.
When is CPT Code 99203 Used?
CPT 99203 is reported when a new patient evaluation includes moderate history-taking, a clinically appropriate examination, and low-level medical decision-making. Under the updated MDM-based rules, the visit typically involves addressing one or two stable medical issues, reviewing limited data such as labs or imaging, and assessing a minimal-to-low risk of complications. Providers commonly use 99203 for evaluations such as new musculoskeletal pain, dermatologic lesions, respiratory infections, stable chronic condition assessments, and referral consultations where the complexity does not rise to the level of 99204.
Claims reviewers confirm that the documentation supports new-patient status, that the complexity aligns with low MDM or 30–44 minutes of total time, and that the service was medically necessary based on the presenting symptoms.
Who bills for CPT Code 99203?
CPT 99203 is billed by physicians and qualified health professionals across nearly every clinical specialty. Primary care physicians, internists, pediatricians, gynecologists, orthopedists, ENT specialists, dermatologists, neurologists, and behavioral health physicians routinely report 99203 when seeing new patients whose conditions require a moderate introductory evaluation. Nurse practitioners and physician assistants also bill 99203 when working within their scope of practice and under payer-recognized NPI structures. Because this code represents one of the most commonly used new patient visit levels, accurate documentation is essential for both compliance teams and provider organizations.
Top Diagnosis ICD-10 for CPT 99203
Although the diagnosis should always reflect the patient’s condition, certain categories frequently align with the complexity requirements of 99203. These include new musculoskeletal complaints, dermatologic evaluations requiring moderate assessment, stable chronic disease reviews, mild respiratory or ENT infections, gastrointestinal symptoms requiring evaluation, and initial behavioral health concerns. Claims reviewers assess whether the diagnosis reasonably requires low-complexity decision-making and whether the documentation supports the clinical reasoning for selecting 99203 over 99202 or 99204. Poor alignment between diagnosis severity and visit complexity is a common reason for payer inquiries.
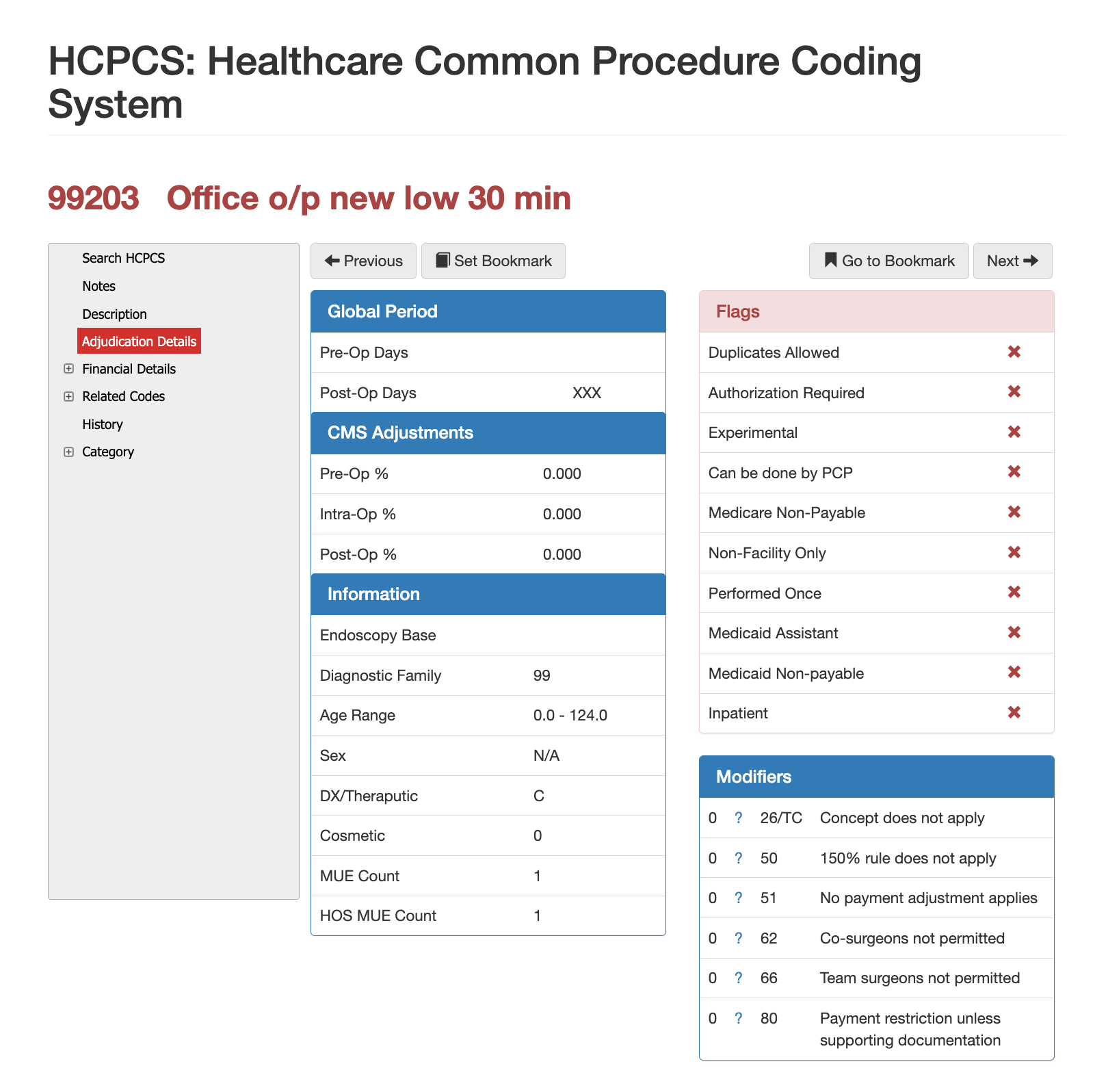
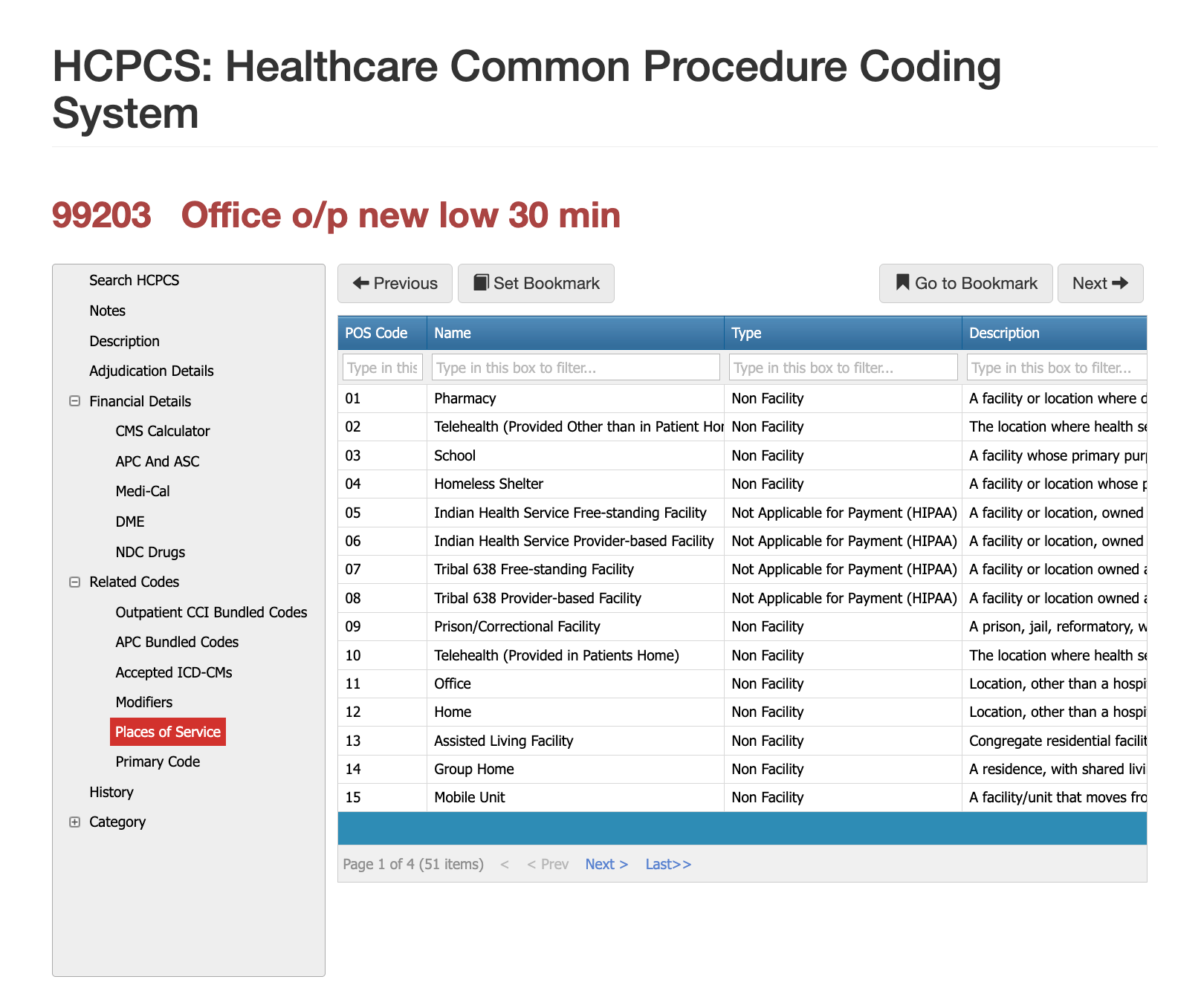
Places of Service for CPT Code 99203
CPT 99203 is most often billed in outpatient settings, including physician offices, urgent care clinics, retail clinics, specialty outpatient departments, and hospital-based outpatient clinics. Although this code represents a new patient evaluation, it is not used for telehealth unless payer rules specifically permit the use of standard E/M codes with modifier 95. Claims reviewers evaluate POS closely because misalignment between service setting and documentation may trigger manual review. For example, reporting a new patient 99203 in a setting where new-patient establishment is not permitted can result in denial.
Proper Documentation for CPT Code 99203
Accurate documentation is fundamental to supporting 99203. Under the updated E/M guidelines, providers must document medical decision-making elements or total time spent. When selecting based on MDM, the note should clearly describe the number and complexity of problems addressed, the amount and type of data reviewed, and risk considerations. When selecting based on time, the provider must document the total time spent in direct and indirect patient care activities occurring on the date of the encounter. The documentation should also confirm that the patient is new to the practice, as established patients require an entirely different E/M code range. Claims examiners frequently deny 99203 when time or MDM criteria are missing or when the medical necessity appears insufficient for the evaluated complexity.
Related CPT Codes for 99203
The primary related codes to a new patient consult (99203 cpt code) is going to be the shorter and longer duration of initial consults (99202, 99204, 99205) and the established patient consults of 99212-99215.
| Code | Description | How It Compares to 99203 |
|---|---|---|
| 99202 | New patient visit, straightforward MDM or 15–29 minutes | Used for simpler evaluations requiring minimal complexity and shorter total time. |
| 99204 | New patient visit, moderate complexity or 45–59 minutes | Represents the next level for more involved assessments or higher MDM complexity. |
| 99212–99215 | Established patient visits | Not used for new patients; incorrect selection is a common billing error. |
Modifier Guidance for CPT Code 99203
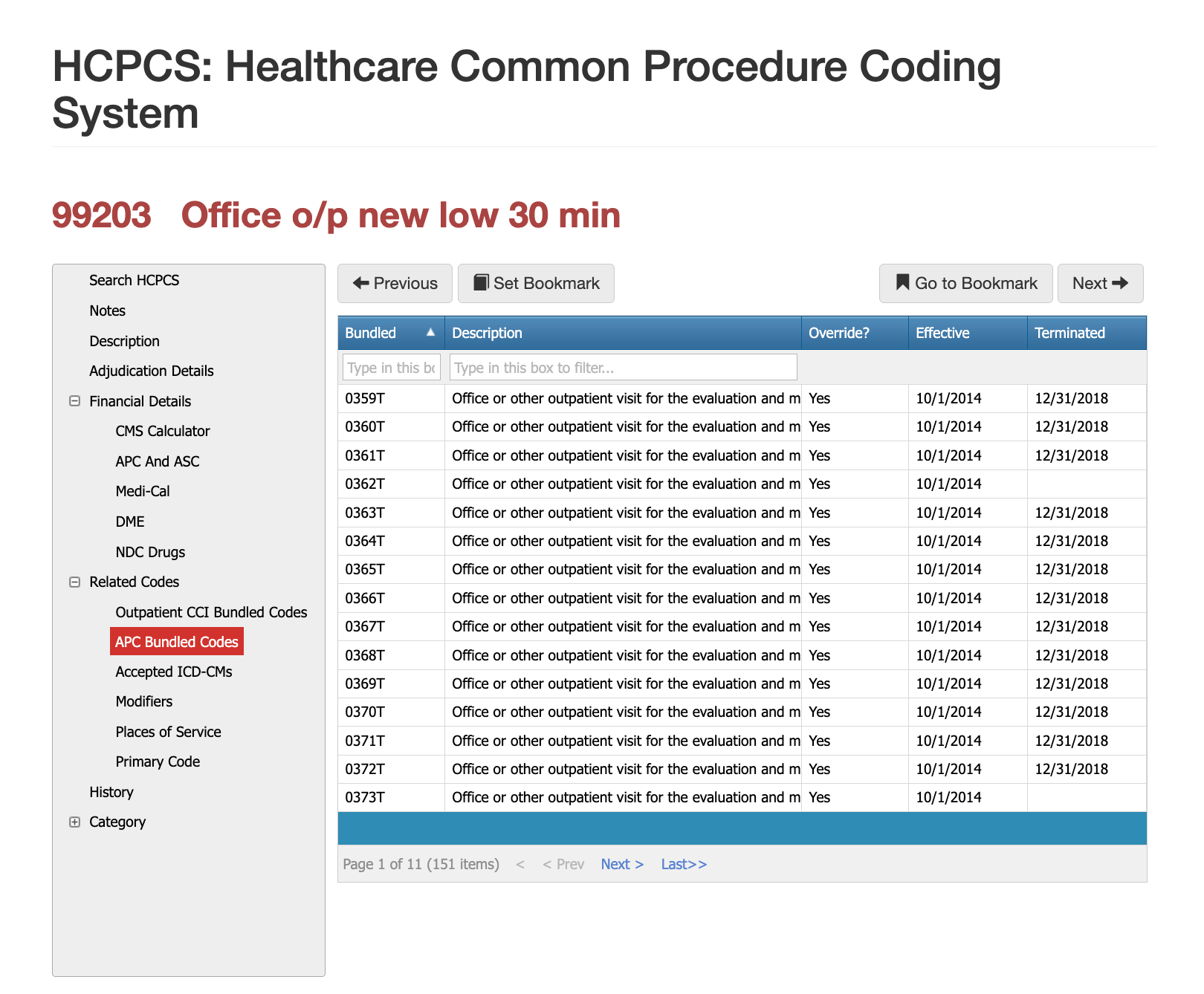
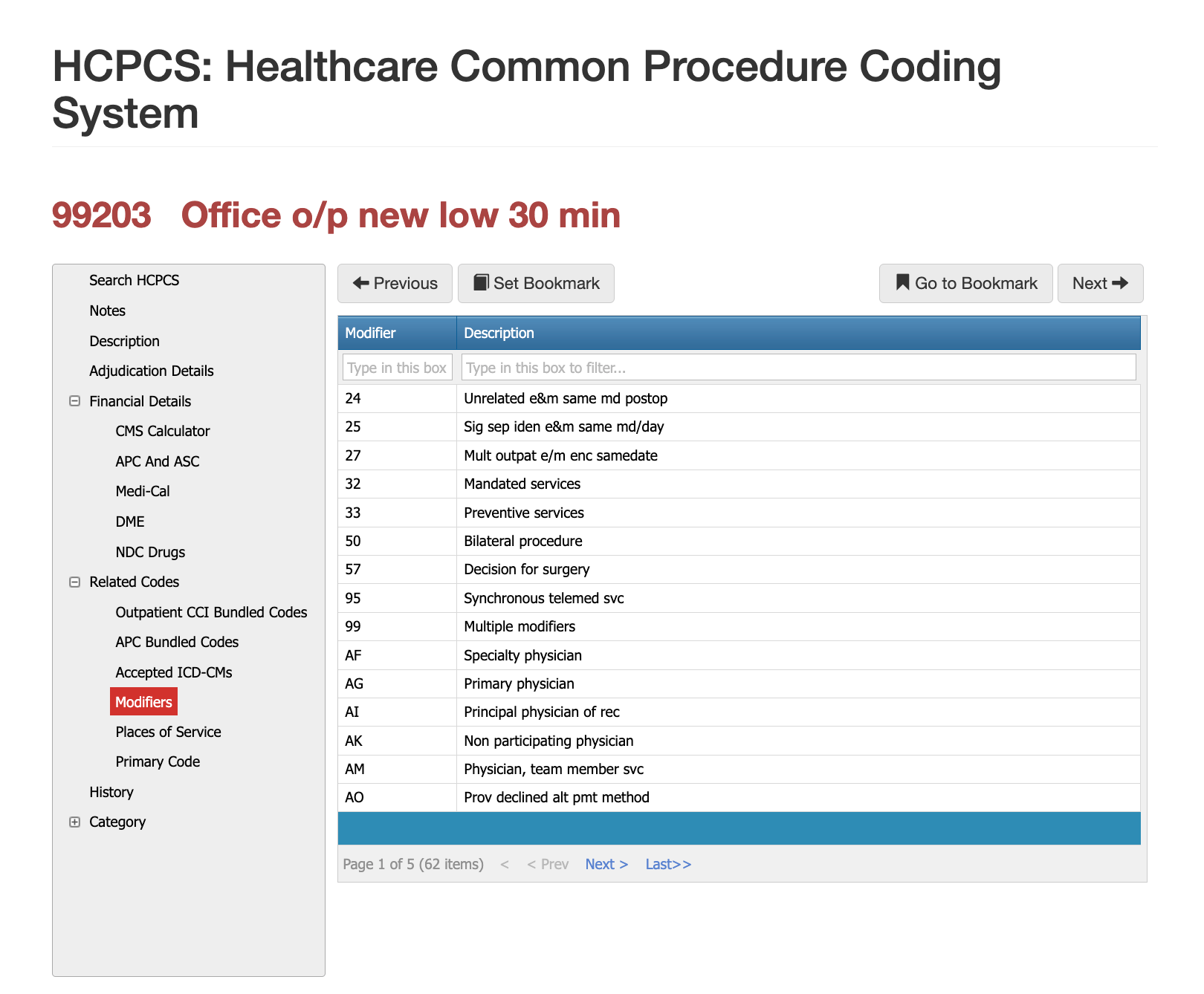
While there are over 60 possible modifiers that could be applied, not all are medically likely dependent upon documentation, place of service of additionally billed procedure or services, so PCG has listed the top three that we have seen in our 30 years of claims auditing below. To get the full list, enroll in iVECoder.
Modifier 25 – Significant, Separately Identifiable E/M Service
Modifier 25 is used when a provider performs a medically necessary procedure on the same day as the E/M visit. The modifier allows 99203 to be billed alongside the procedure, provided the E/M service addressed a different or additional clinical concern beyond the decision to perform the procedure. Claims examiners often deny modifier 25 when the documentation reads like a routine pre-procedure evaluation rather than a separate, substantive service.
Modifier 95 – Synchronous Telemedicine Service
Modifier 95 may be used when payer rules allow 99203 to be delivered via real-time telehealth. Documentation must identify the modality, confirm patient consent, and ensure the complexity level is appropriate for virtual care. Some payers restrict telehealth use of new-patient E/M codes, making policy review essential.
Modifier 33 – Preventive Service
Modifier 33 is occasionally appended when payers classify certain evaluations as preventive under specific circumstances. This is rare for 99203 but may appear when preventive elements overlap with problem-oriented care and payer rules permit such classification.
Most Common Reasons for 99203 CPT Denials
Payers most frequently deny 99203 when documentation does not support the level of medical decision-making or the time requirement is missing. Denials also occur when the diagnosis does not align with the complexity of the visit, when the provider incorrectly uses the code for an existing patient, or when modifier 25 is misapplied without clearly distinct E/M work. Inconsistent time entries, conflicting exam details, or incomplete new-patient documentation often lead to post-payment review or claim downcoding to 99202. Here's three scenarios we've seen a lot in our 30 years of claims auditing.
The 3-year Requirement
As a provider you can only bill a 99203 every three years of continous care. We've seen providers who have seen a patient 10-24 months in duration or 1-3 times and still try to bill a 99203. This is incorrect, this is an established patient for each 3-year span.
Handing off patients to Mid-Levels
When a clinic's MD establishes an initial 99203, the mid-level who bills under that MD as well as all other MDs within that specialty and that billing ID / Clinic may not bill a 99203 until the 3-year period has been reached.
Duplicate Global Period Billing
When a provider has both a hospital position and an outside clinic, the billing ID may be different but that patient is still their established patient. We have seen both outpatient first and hospital first 99203 and then later billed at the other location (POS) which violates the 3-year requirement.
Multiple Locations Same Billing ID
In our 30 years, PCG has seen a Provider (Dr. Jones) who serves multiple locations under the same organization. As he moves from one location to the next, the patient may be seen at multiple locations by him and/or his mid-levels, but this is not a 99203. Changing location doesn't warrant a new 99203 charge, it is instead a 99213.
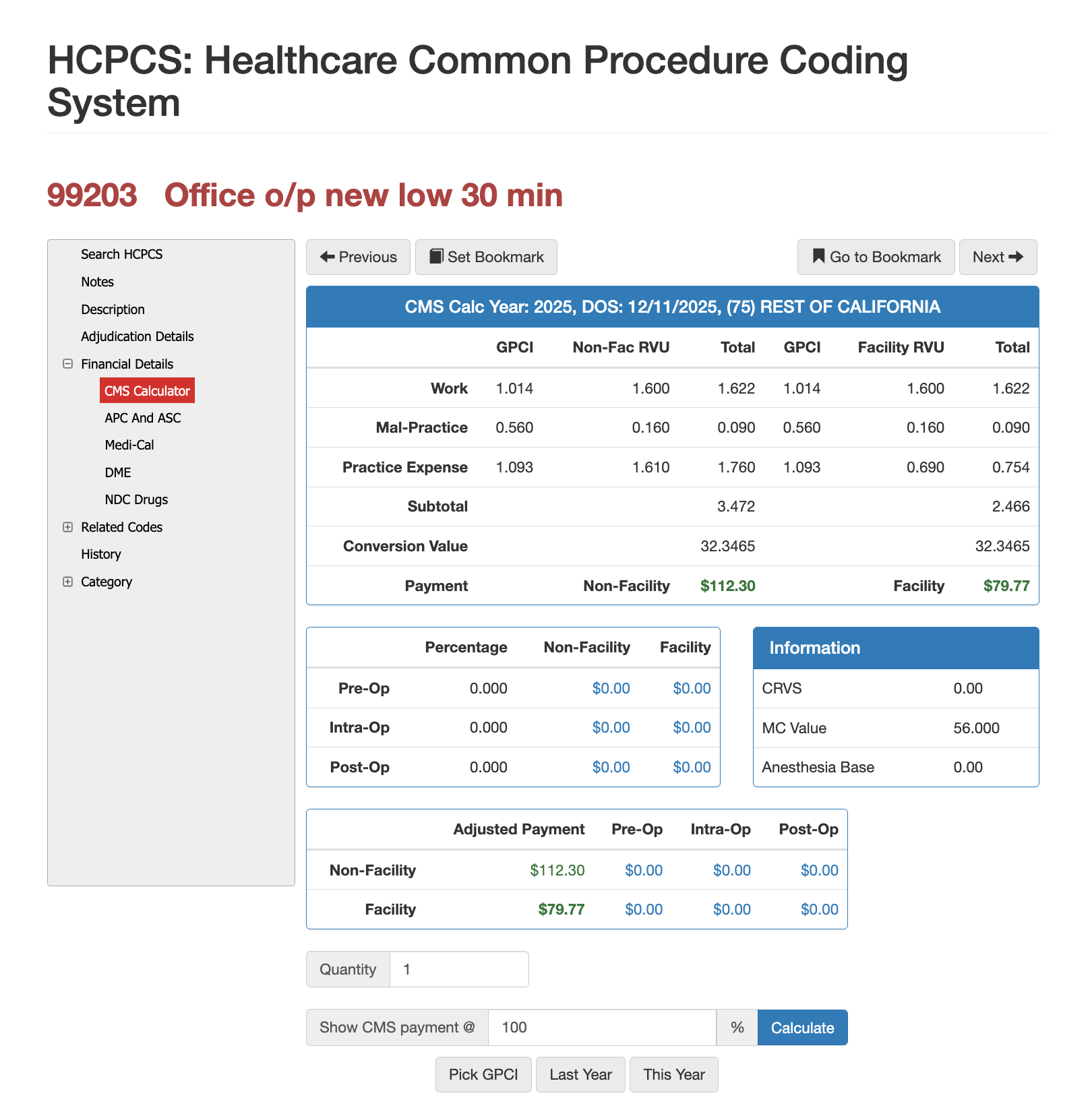
RVUs and Financials for CPT Code 99203
RVU Negotiation Guide for CPT 99203
Reimbursement for 99203 is driven by its relative value units (RVUs), which include work, practice expense, and malpractice components. Final payment varies based on geographic practice cost indices (GPCI), payer contractual adjustments, and whether the service was performed in a facility or non-facility setting. Providers often analyze 99203 payment trends when negotiating payer contracts, as the code sits at a high-volume utilization point for outpatient practices. Using Virtual AuthTech or iVECoder enables both payer and provider organizations to simulate reimbursement rates at various Medicare percentages, evaluate financial outcomes across states, and ensure fee schedules appropriately match the true value of low-complexity new-patient care.
The Easier Way to Research codes
For more than 30 years, PCG Software has supported Health Plans, MSOs, IPAs, TPAs, and provider organizations in improving coding accuracy, strengthening compliance, and reducing fraud, waste, and abuse. Our solutions, including Virtual Examiner®, VEWS™, and iVECoder®, are built on decades of payer-side adjudication experience and reflect the same logic used by health plans nationwide. National regulatory guidance, payer policies, compliance standards, and large-scale claims review patterns inform this CPT 69210 analysis.
Toss out the CPT book.
Stop researching articles.
Sign up for iVECoder today!
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others