CPT Code 88365 Definition, Usage, and Scenarios
CPT Code 88365 - Level IV Pathology Summary
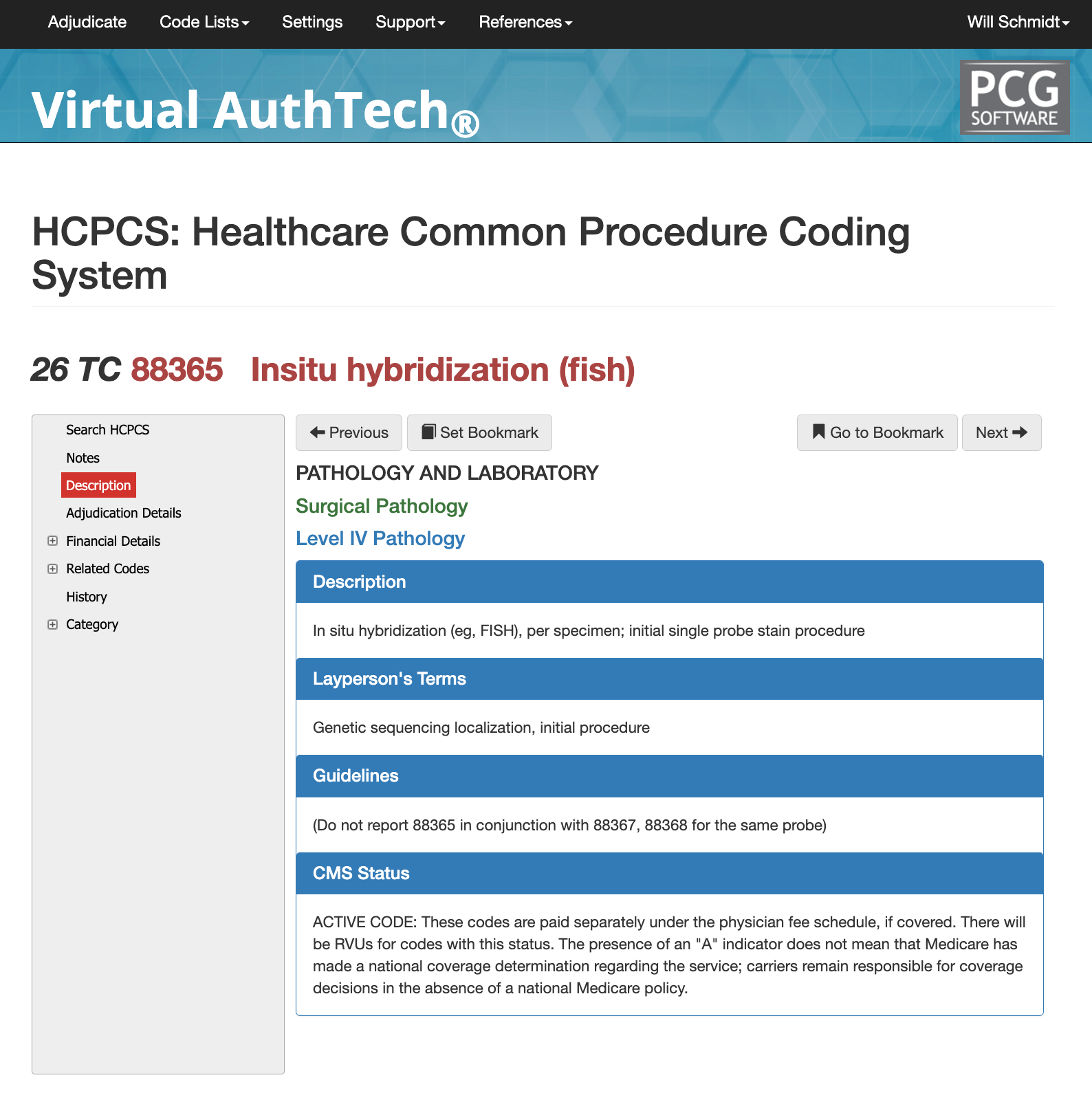
Learn about CPT Code 88365, a Level IV pathology HCPCS commonly used for in situ hybridization (e.g., FISH) per specimen, particularly for the initial single probe stain procedure. This code is critical in genetic sequencing localization and plays a key role in surgical pathology. In this article, we’ll dive deep into the details of this code, including its guidelines and coverage considerations. You’ll also discover how AI code scrubbers can ensure accuracy, streamline coding efficiency, and maintain compliance within your pathology practice.
What and when do you use cpt code 88365
What Providers bill 88365 the most?
CPT 88365 is primarily billed by
pathologists,
molecular pathology laboratories, and
cytogenetic laboratories performing advanced diagnostic testing. Hospital-based surgical pathology departments and independent molecular diagnostic labs also routinely report 88365, especially in oncology settings where FISH testing is used to evaluate breast cancer markers, hematologic malignancies, and solid tumor genetics. While ordering clinicians include oncologists, hematologists, obstetricians, and surgeons, billing for 88365 is almost always performed by the interpreting pathology laboratory, not the treating provider. Medicare and commercial payers reimburse this code consistently when the test is clinically indicated and supported by diagnostic pathology guidelines.
Proper Documentation for getting 88365 Approved
Accurate reporting of 88365 requires documentation that clearly identifies the specimen, the purpose of testing, and the specific probe used. The pathology report must describe the hybridization procedure, findings, interpretation, and clinical relevance. For FISH testing, documentation should include signal patterns, control validation, and correlation with morphologic or clinical data. Missing elements—such as failing to specify the probe used, omitting the diagnostic rationale, or not linking the test to a medical necessity indication—are common reasons for payer denials. Thorough documentation improves compliance and supports reimbursement, particularly when multiple probes or add-on codes are involved.
When 88365 May Be Reported with an E/M Code
88365 may be billed with an E/M service only in rare circumstances where a pathologist provides a separately identifiable, medically necessary consultation beyond test interpretation. More commonly, 88365 is paired with appropriate add-on codes (e.g., 88364, 88367, 88368) when additional probes or automated analysis are performed. Each code must reflect the specific technical and interpretive components provided. When multiple related molecular tests are conducted on the same specimen, the pathology report must clearly differentiate each service to avoid bundling edits.
Crisis or Emergency scenarios for 88365
While CPT 88365 is not a “crisis” code, it is frequently used in
urgent diagnostic scenarios, such as rapid evaluation of suspected leukemias, lymphomas, congenital abnormalities, or high-risk oncologic conditions where immediate genetic clarification influences treatment decisions. In these cases, the CPT code remains 88365 for the initial probe, but documentation should reflect the
clinical urgency, the
specific diagnostic question, and the
reason rapid FISH testing was medically necessary. This helps prevent medical necessity denials, especially when expedited testing incurs higher cost or faster turnaround time requirements.
Adjudication Details for CPT 88365
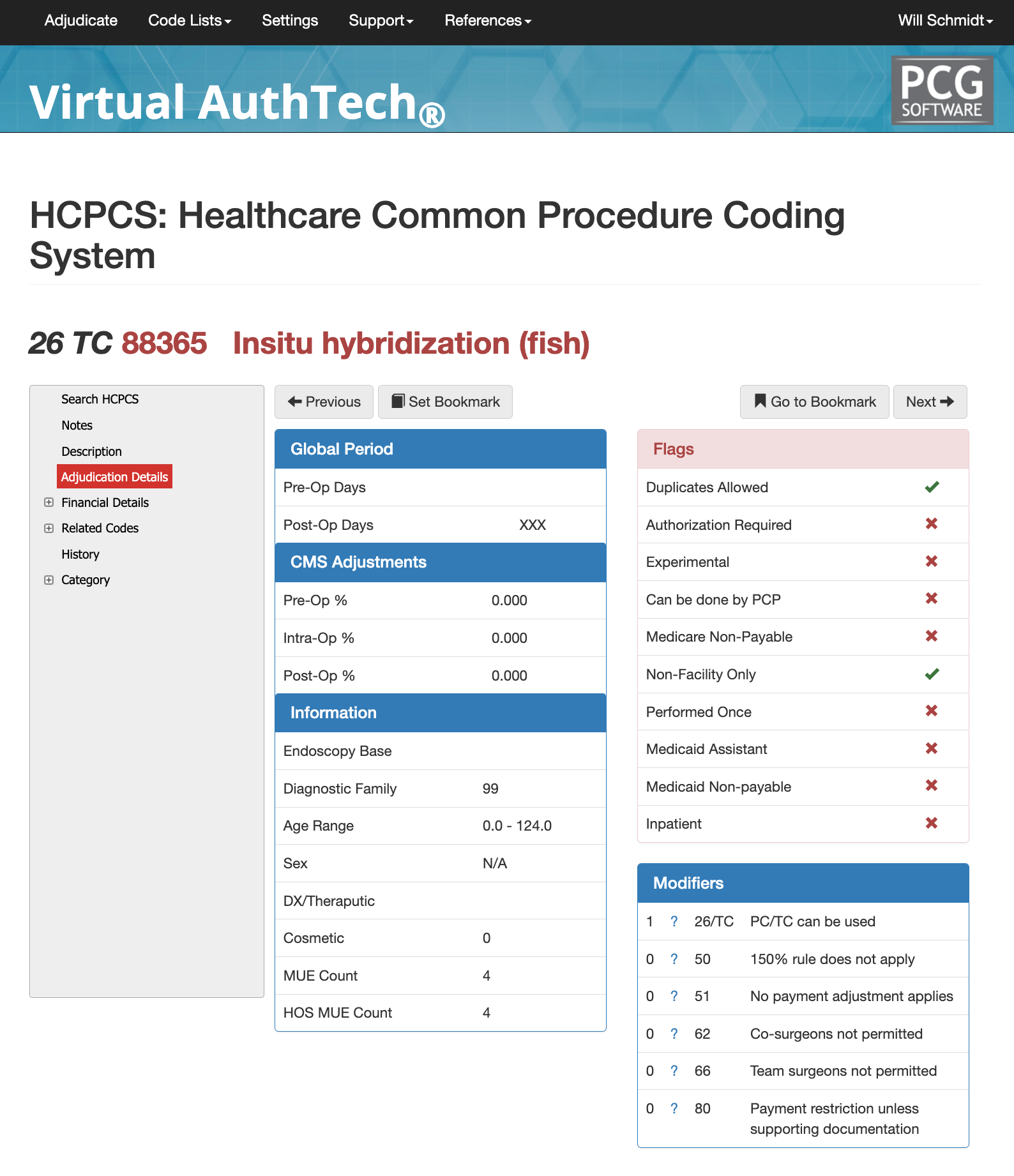
88365 CPT Adjudication Description and Guides
88365 cpt code has a diagnostic family of 99, with no age range, and has an MUE Count of “4”, and HOS MUE Count of “4", and this code should be billed in a Non-Facility Only setting (POS).
There are 14 Outpatient CCI Bundled Codes that could apply, so make sure you use iVECoder or VirtualAuthTech to properly select the right bundled code. Remember that unbundling codes leaves your payer organization and/or clinic up to fines and possible reimbursement decreases due to incorrect encounter data.
Adjudication Details for CPT Code 88365
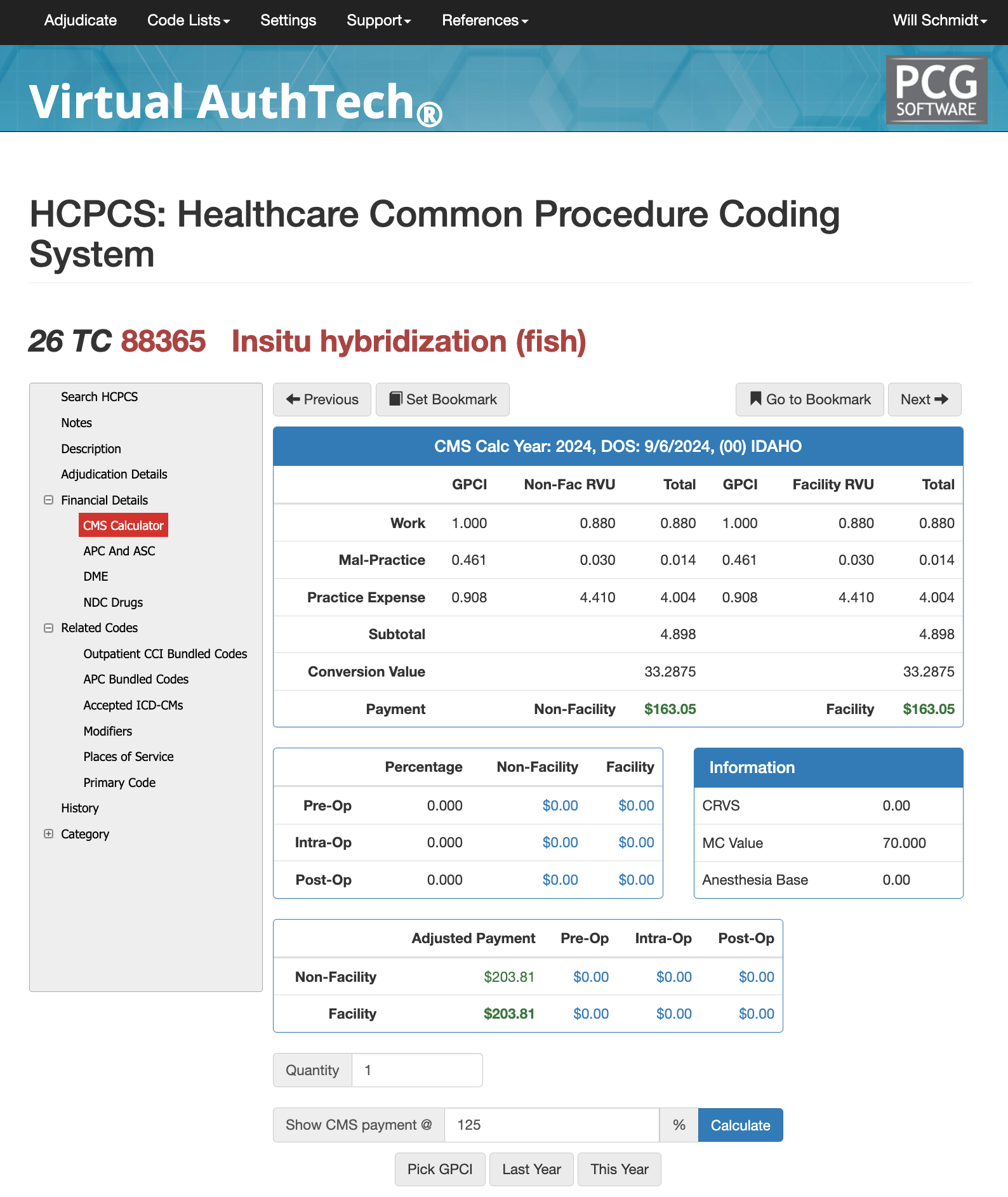
By using an iVECoder or Virtual AuthTech, you can also set your GPCI, then dive deeper into the specific code (88365 cpt) to see what the 100% to CMS payment is, and then alter the "show cms payment @" section to calculate 125% or higher to help negotiate the best rates. Additionally, it will show both the non-facility versus facility rates, further helping you with your DOFRs.
CPT Code 88365 Bundled Codes and Modifiers
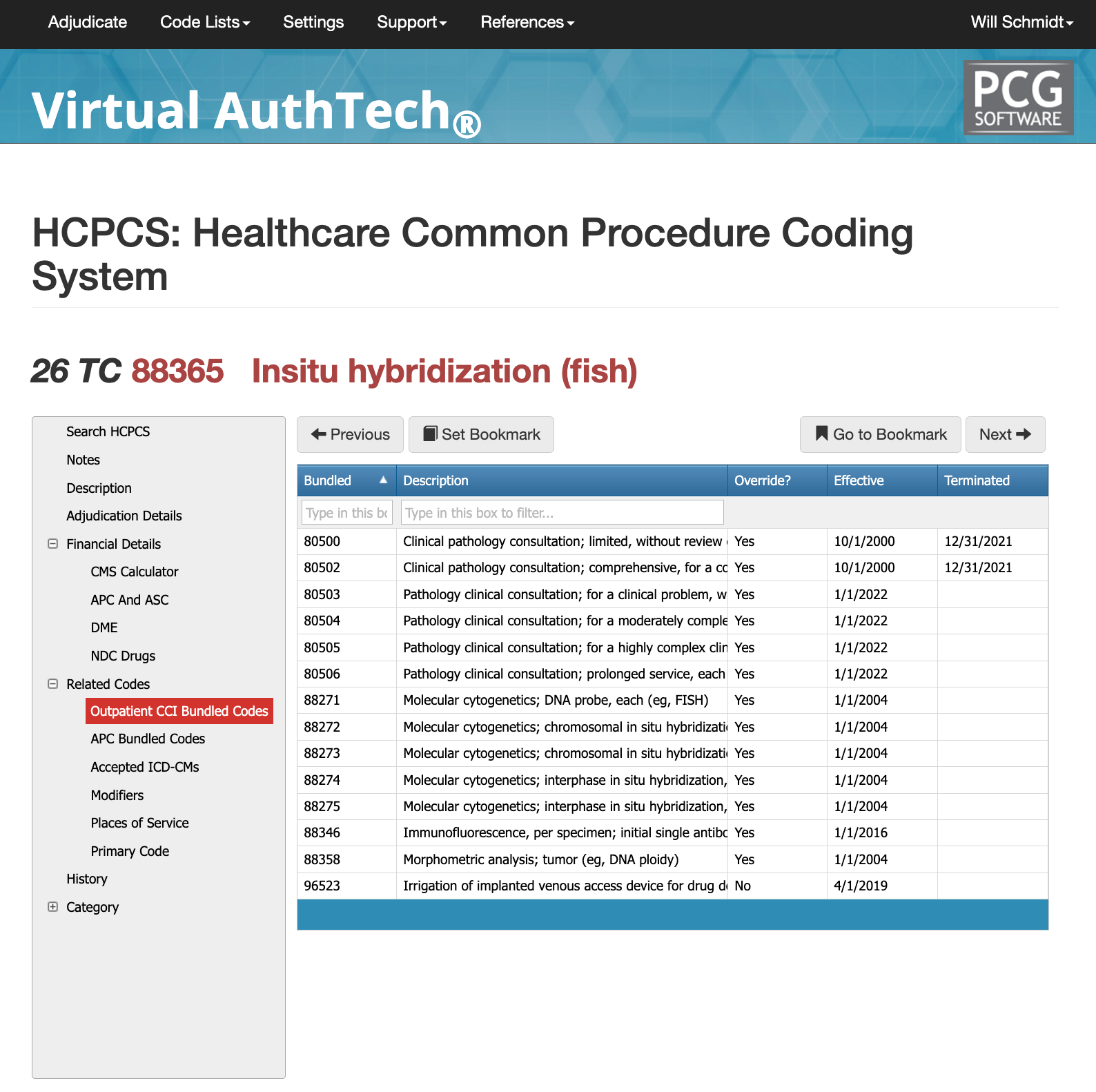
CPT 88365 is often reviewed under National Correct Coding Initiative (CCI) bundling rules because in situ hybridization is commonly performed along with other pathology tests. When a FISH test is done on the same specimen as routine histology,
immunohistochemistry, or other molecular studies, payers may consider parts of the work overlapping. In these cases, certain services may be bundled together, meaning only one code is allowed unless documentation clearly shows that each test served a different diagnostic purpose. Add-on codes for extra probes or automated analysis can be reported when they truly represent additional work, but they cannot be billed if only the initial probe is used.
In hospital outpatient settings, 88365 may also be bundled under APC payment rules, especially when the test is considered part of a larger diagnostic encounter. This means the laboratory may not receive separate payment even though the service was performed. Using an auditing tool such as Virtual AuthTech helps laboratories review bundling rules in advance, confirm which codes can be billed together, and avoid denials caused by missing or unclear documentation.
Places of Service for CPT Code 88365
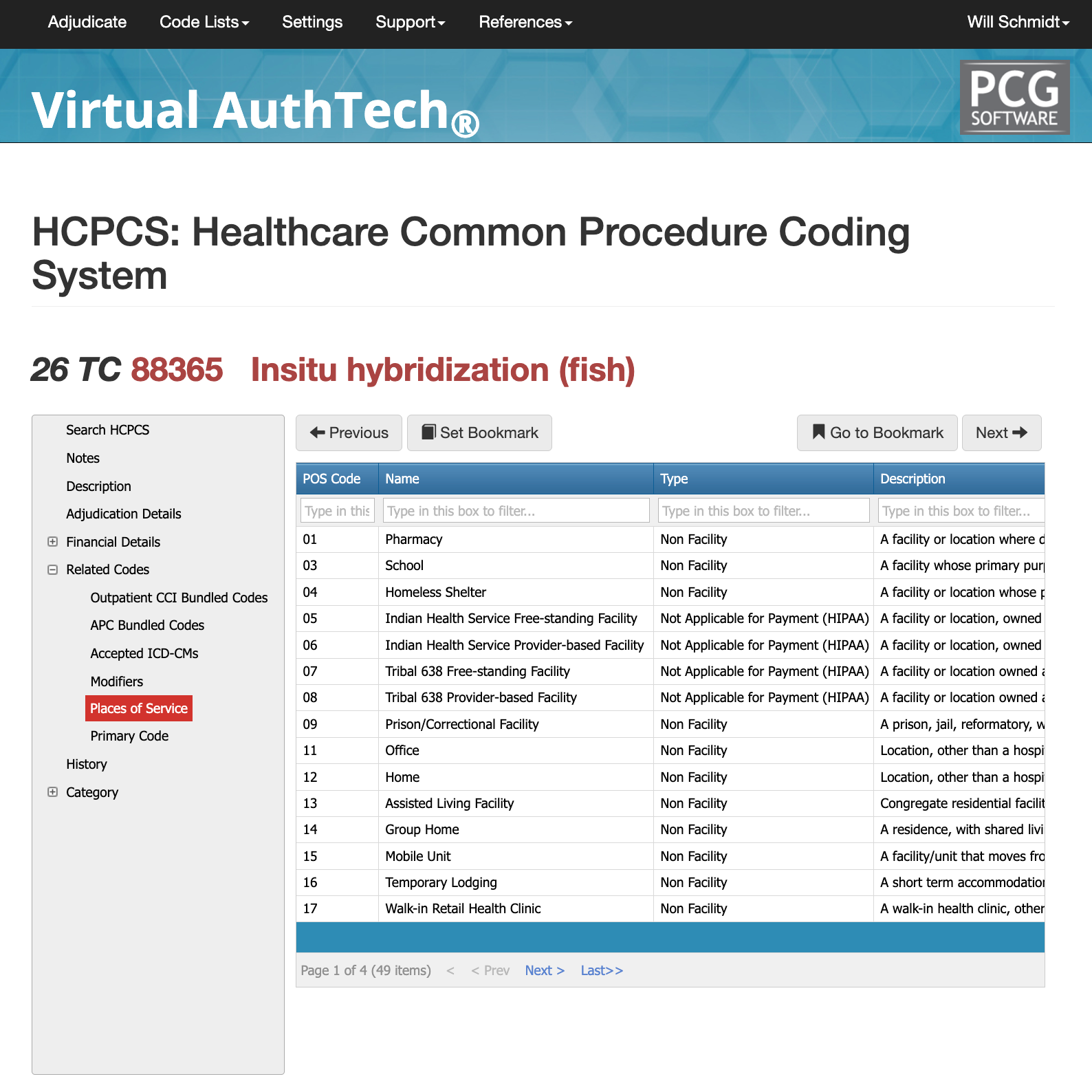
There are 49 current POS that could be used, ranging from Pharmacy (01), Homeless Shelter (04), Assisted Living (13), Walk-In Retail Health Clinic (17), Urgent Care (20), and Inpatient Hospital (21), among others. To get the complete listing, enroll
IVECoder for Clinics or VirtualAuthTech for Payers.
Most commonly used modifiers for 88365 CPT
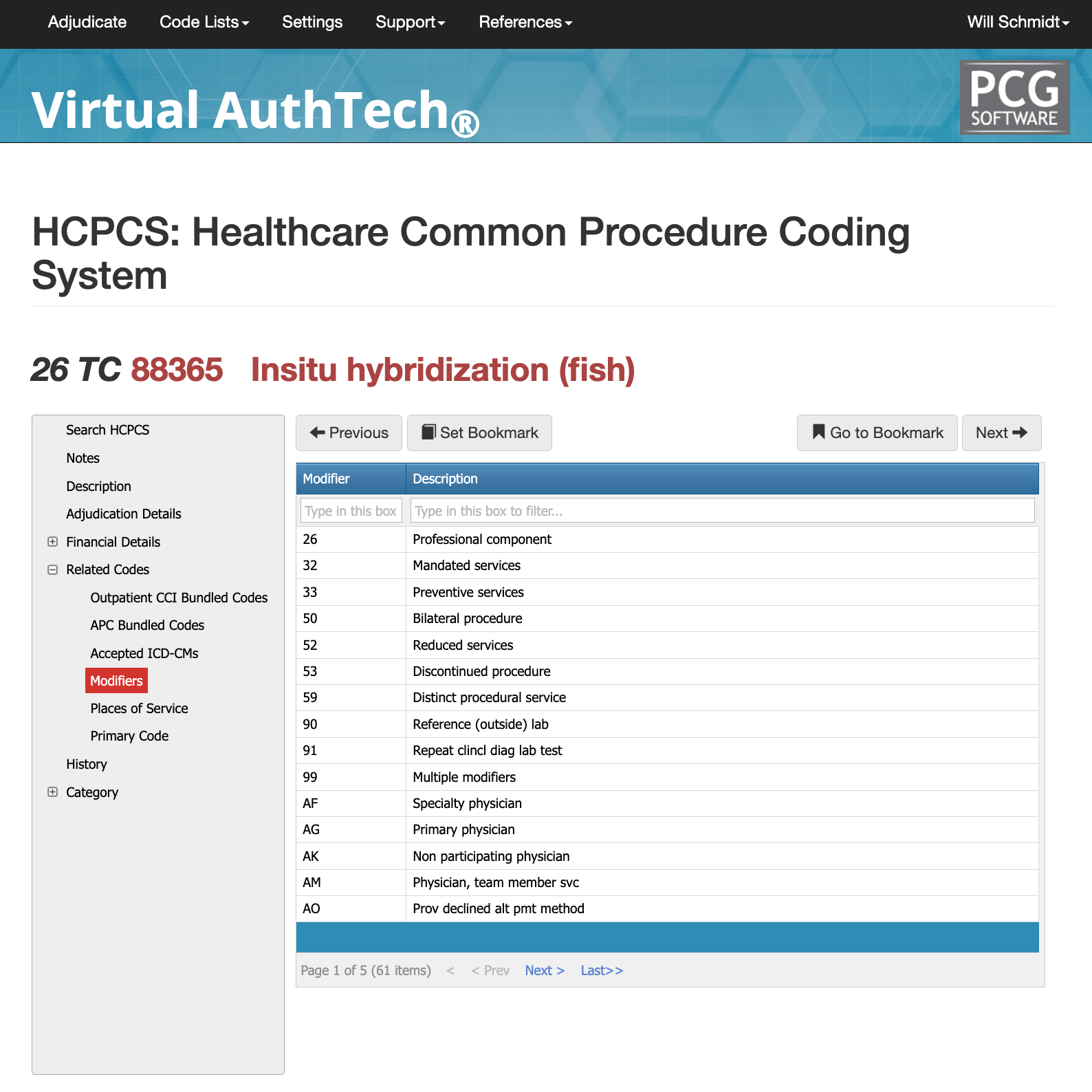
There are more than 60 modifiers that may be used with CPT 88365, depending on how the pathology service was performed and what portion of the work the laboratory is billing for. The most commonly used modifiers include
26 for the professional component,
33 for preventive services,
50 for bilateral procedures,
59 for distinct procedural services, and specialty-based modifiers like
AF and
AG. Most pathology labs use only a small number of these modifiers regularly, but choosing the wrong one can lead to denials. Below are the three modifiers most commonly associated with CPT 88365 and why they are used.
Modifier 26 with CPT Code 88365
Modifier 26 is used when the pathologist is billing
only the professional interpretation of the test and not the technical laboratory work. This commonly applies when a hospital or outside reference lab performs the staining and hybridization, but the pathologist provides the diagnostic interpretation and report. Using modifier 26 clearly tells the payer that the claim represents interpretive work only. If both the technical and professional components are performed by the same laboratory, modifier 26 should not be used.
Modifier 59 with CPT Code 88365
Modifier 59 is used when CPT 88365 is performed as a
separate and distinct service from other pathology procedures done on the same specimen. Because molecular, cytogenetic, and histology tests often overlap, payers may bundle services unless documentation shows a clear, separate diagnostic purpose. Modifier 59 helps prevent automatic denials by indicating that the FISH test addresses a different clinical question than the other tests performed. To use this modifier correctly, the pathology report must explain why the hybridization study was necessary and how it differs from the other diagnostic work.
Modifier 33 with CPT Code 88365
Laterality modifiers are essential when billing unilateral joint injections. RT indicates the right side and LT indicates the left side. When a provider performs injections in two different joints on opposite sides of the body—such as the right knee and left shoulder—each line item must reflect the correct RT/LT designation. Many Medicare contractors prefer RT/LT for bilateral claims instead of modifier 50, so payer policy review is required.
PCG Software’s Authority and Expertise in CPT Code Interpretation
For more than 30 years, PCG Software has supported payers, MSOs, IPAs, TPAs, and clinical organizations in improving claims accuracy, preventing fraud and waste, and strengthening compliance around high-volume procedure codes such as 20610. Our solutions—including
Virtual Examiner®,
VEWS™, Virtual AuthTech, and
iVECoder®—apply payer-side adjudication logic, NCCI rules, and multi-year episode-of-care analytics to identify coding errors before payment is released. By combining clinical insight with rule-based automation, PCG helps organizations reduce improper payments, enhance operational efficiency, and maintain full compliance across musculoskeletal and orthopedic claims workflows.
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others