CPT 57410 - Cervical Biopsy with Endocervical Curettage
How to get more approvals with CPT Code 57410
CPT Code 57410 describes a cervical biopsy performed with endocervical curettage during the same encounter. Gynecologists use this code when evaluating abnormal Pap smears, HPV-related lesions, unexplained bleeding, infectious changes, or when screening for precancerous or malignant cervical disease. In this article, we cover AMA and layperson definitions, documentation requirements, diagnoses that support medical necessity, place-of-service rules, modifiers, bundling considerations, and financial insights for both payers and providers. You will also learn how tools like Virtual Examiner and iVECoder ensure accurate billing and reduce common claim denials.
The Who, What, When for billing and paying for CPT Code 57410
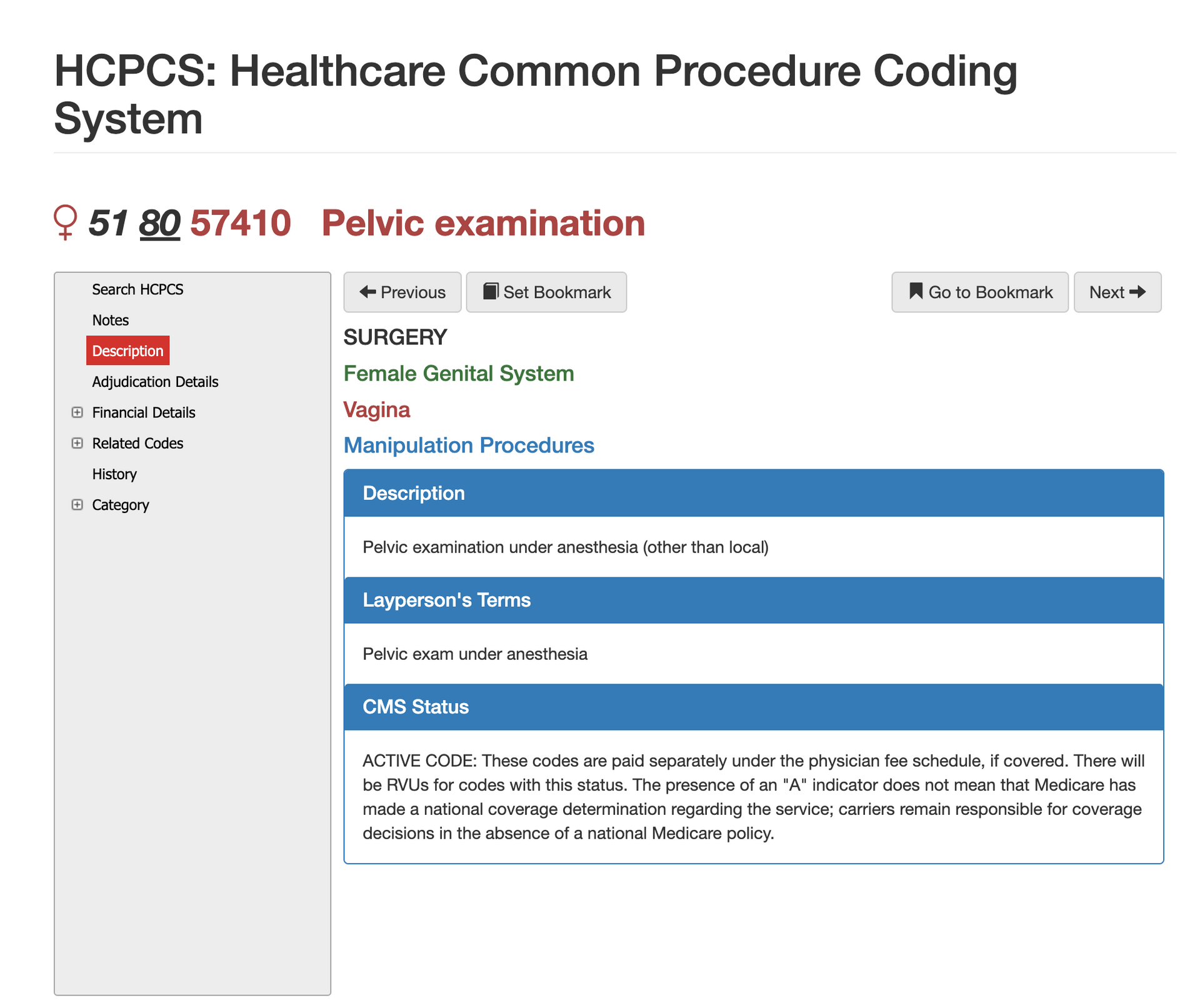
Definition of CPT Code 57410 - AMA vs Layperson:
The AMA defines CPT Code 57410 as “Biopsy of cervix, single or multiple, with endocervical curettage.” In everyday terms, this procedure involves removing tissue from the cervix and scraping cells from the endocervical canal for microscopic evaluation. It is more extensive than a simple cervical biopsy because the curettage component examines cells deeper inside the cervical canal. Clinicians perform this procedure when screening for infection, dysplasia, HPV-related changes, or cervical cancer, and payers expect documentation to reflect why both tissue types were necessary for diagnosis.
When is CPT Code 57410 Used?
CPT 57410 is appropriate when a gynecologist evaluates cervical tissue through biopsy
and obtains additional endocervical samples through curettage. This code is commonly used following abnormal Pap results, high-risk HPV findings, unexplained vaginal bleeding, visible cervical lesions, or concerns for neoplasia. Because the biopsy and curettage are combined into one code, providers should not bill separate biopsy or curettage codes unless documentation clearly supports distinct, medically necessary work. Claims examiners look closely at procedure notes to verify that both components—biopsy and curettage—were performed during the encounter.
Who bills for CPT Code 57410?
CPT 57410 is primarily billed by OB/GYN physicians during in-office diagnostic evaluations. However, family physicians, women’s health practitioners, and advanced practice providers such as nurse practitioners and physician assistants may also perform and bill this service when scope-of-practice rules allow. Hospital outpatient departments may submit the technical component when the procedure occurs in a facility setting. Because cervical biopsies are one of the most common gynecologic diagnostic procedures, CPT 57410 is widely recognized and reimbursed by Medicare, Medicaid, and commercial payers when documented appropriately.
Top Diagnosis ICD-10 for CPT 57140
Diagnoses supporting CPT 57410 typically relate to cellular abnormalities, HPV positivity, cervical lesions, infections, or unexplained gynecologic symptoms. Common ICD-10 categories include cervical dysplasia (N87 codes), abnormal Pap results (R87 series), high-risk HPV (B97.7), post-coital bleeding, and suspicious gynecologic symptoms requiring tissue sampling. Claims are often denied when the diagnosis suggests a minor or unrelated issue that does not warrant invasive evaluation. Linking clinical findings directly to the need for biopsy and curettage ensures medical necessity is clear.
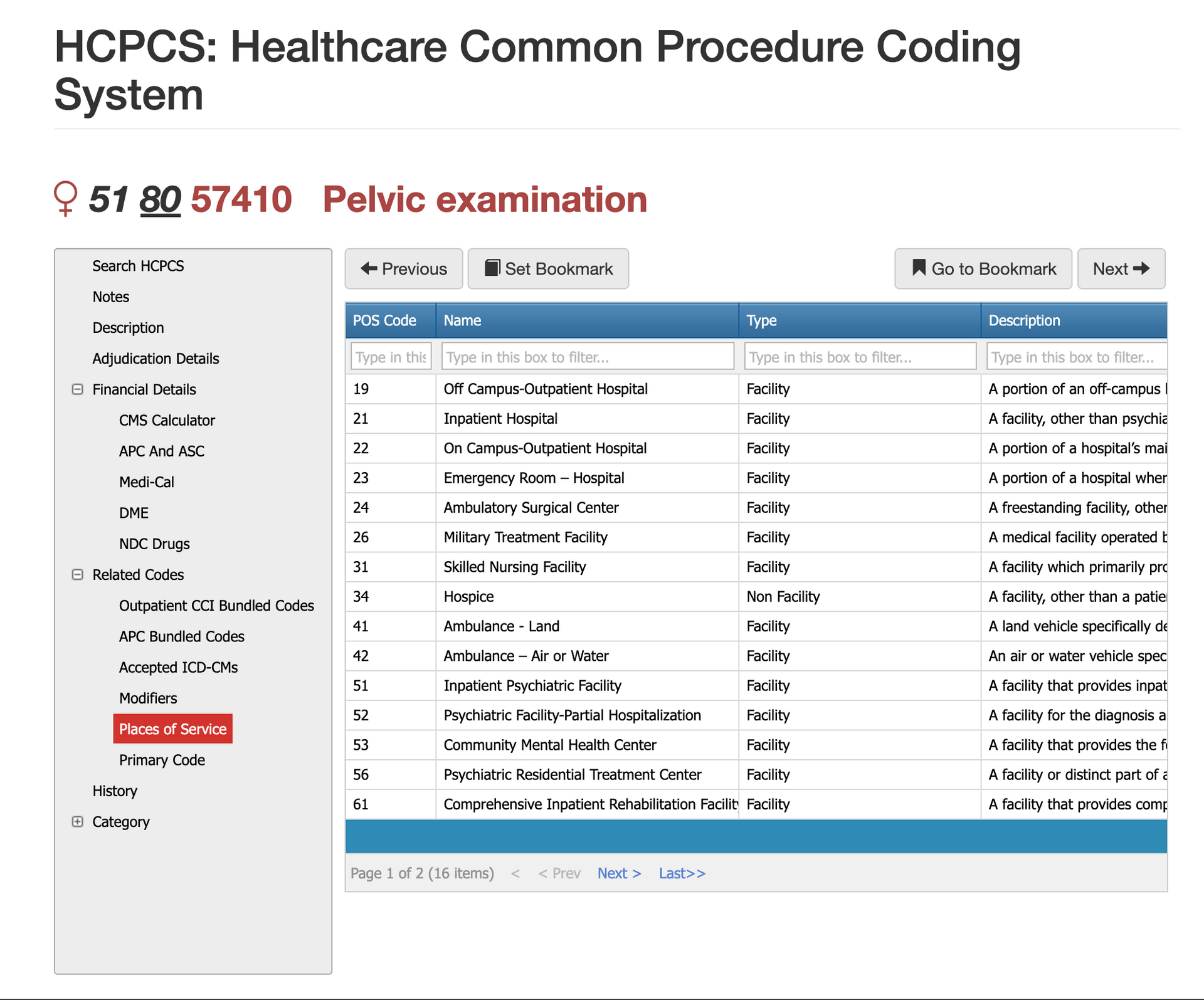
Places of Service for CPT Code 51740
CPT 57410 is performed most frequently in
office settings (POS 11), where gynecologists conduct routine diagnostic evaluations. It may also be billed in
hospital outpatient departments (POS 22) or
ambulatory surgical centers (POS 24) when pathology risk, anesthesia needs, or complex findings require a controlled environment. Because this is a minor diagnostic procedure, inpatient claims are rare unless performed incidentally during hospitalization for unrelated conditions.
Proper Documentation for CPT Code 20220
Clear and complete documentation is essential to support CPT 57410. The medical record should include the indication for the biopsy—such as abnormal cytology, high-risk HPV, visible lesions, or persistent bleeding. Providers must document both the cervical biopsy technique and the endocervical curettage, including the type of instrument used, the number of samples obtained, and any complications or patient responses. The pathology submission should be referenced, and the note should reflect clinical findings that justify why tissue from both the cervix and endocervical canal was required. Missing documentation of either component is one of the most common denial triggers.
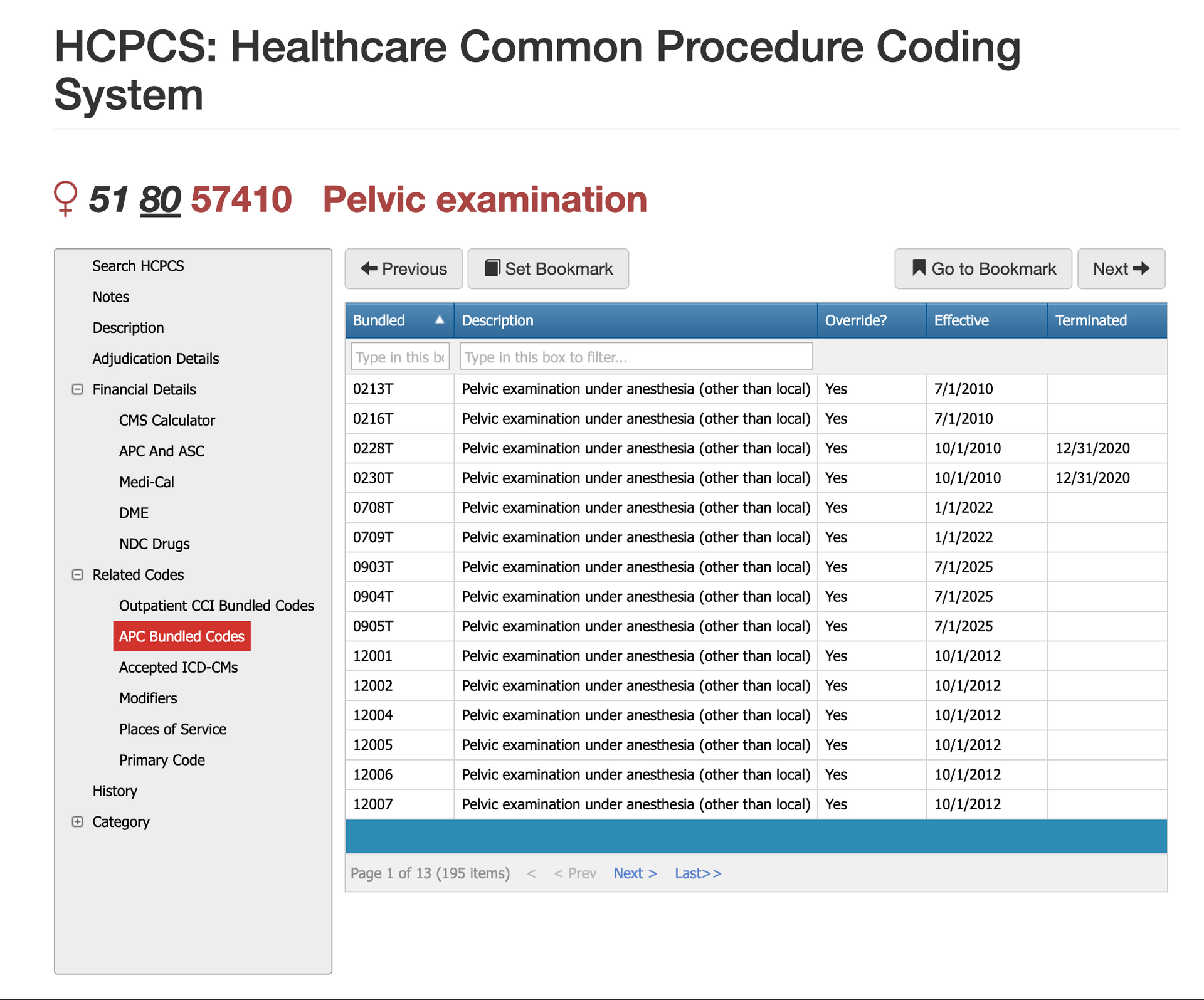
Bundled Codes for CPT Code 51740
CPT 57410 interacts with several bundling rules, especially when performed alongside pelvic examinations, colposcopy, or other gynecologic procedures. Under CCI edits, many diagnostic pelvic services bundle into 57410 unless documentation supports separate, medically necessary work. Colposcopy codes in the 57420–57454 range often replace or bundle with 57410 unless clearly distinct. Providers should not separately report endocervical curettage or superficial biopsies, as these services are already included in the primary code. Claims examiners frequently deny 57410 when unbundled services appear on the same claim without justification.
Related CPT Codes for 51740
Below you will find the most common related codes to CPT 51740, but not all codes. To access all codes, consider
iVECoder for quick search and research capabilities.
| CPT Code | Descriptor | How It Differs From 57410 |
|---|---|---|
| 57410 | Cervical biopsy with endocervical curettage | Base code for combined biopsy and ECC. |
| 57454 | Colposcopy with biopsy + ECC | Includes colposcopy; replaces 57410 when performed. |
| 57500 | Cervical biopsy, not otherwise specified | Does not include curettage; less comprehensive. |
| 57505 | Endocervical curettage alone | Curettage only; used when no biopsy is taken. |
| 57420 | Colposcopy with biopsy | Includes colposcopy but not ECC unless specified. |
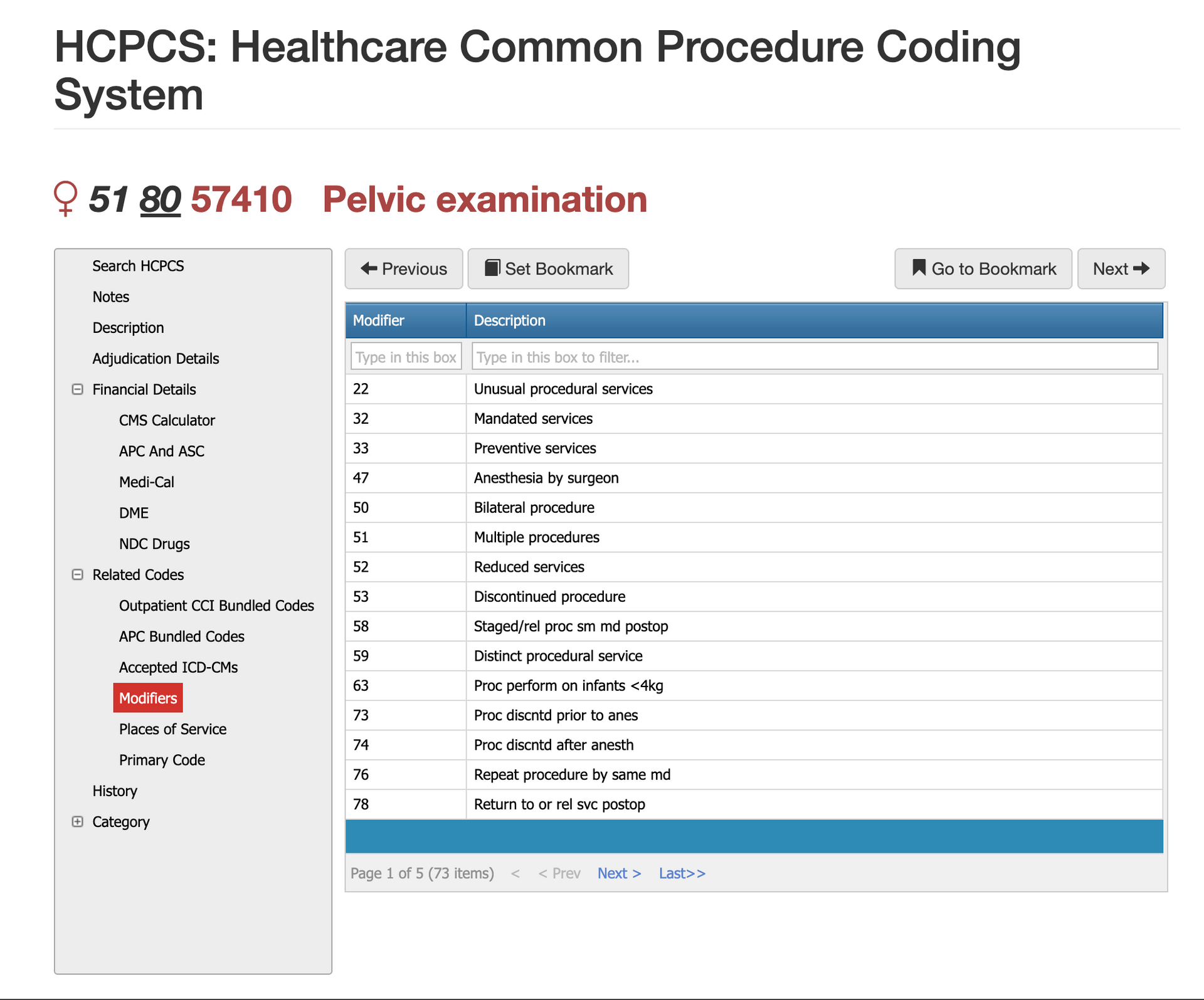
Modifier Guidance for CPT Code 51740
Modifiers help clarify whether the biopsy and curettage were performed under special circumstances or alongside other gynecologic procedures.
Modifier 25 for CPT Code 51740
Modifier 25 applies when an evaluation and management service is performed in addition to the biopsy and curettage. The E/M must address a distinct set of medical concerns, and documentation must clearly separate decision-making from the procedure itself.
Modifier 59 for CPT Code 51740
Although the cervix is a midline structure, some payers require anatomical clarity when procedures occur alongside other pelvic services. RT/LT is rare for 57410 but may be used when bundled with procedures involving paired organs.
Modifier RT/LT for CPT Code 51740
Modifier 59 is used when the superficial bone biopsy is separate and distinct from another procedure performed on the same day. This may apply when the biopsy is taken from a different anatomical site or when it is clinically independent of the primary service. Examiners look for clear documentation that the biopsy was not an integral or bundled part of another musculoskeletal procedure.
Most Common Reasons for 51740 CPT Denials
Claims for CPT 57410 are commonly denied when documentation does not clearly confirm both a cervical biopsy and an endocervical curettage were performed. Denials also occur when diagnosis codes do not support medical necessity, when colposcopy is billed inappropriately with 57410, or when payers detect bundling conflicts under CCI edits. Claims submitted without clear pathology documentation or without specifying the clinical indication often trigger manual review.
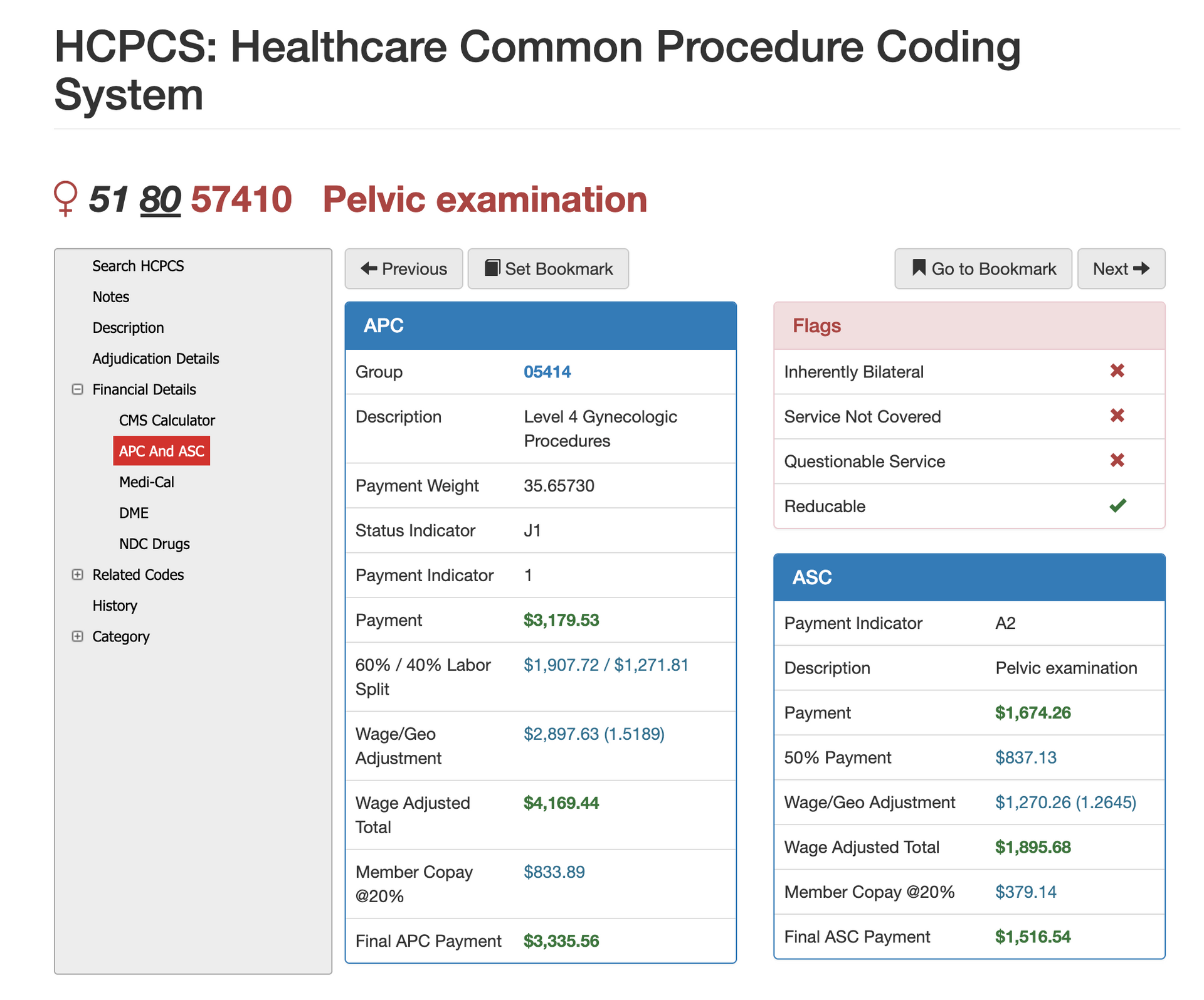
RVUs and Financials for CPT Code 20220
RVU Negotiation Guide for CPT 57410
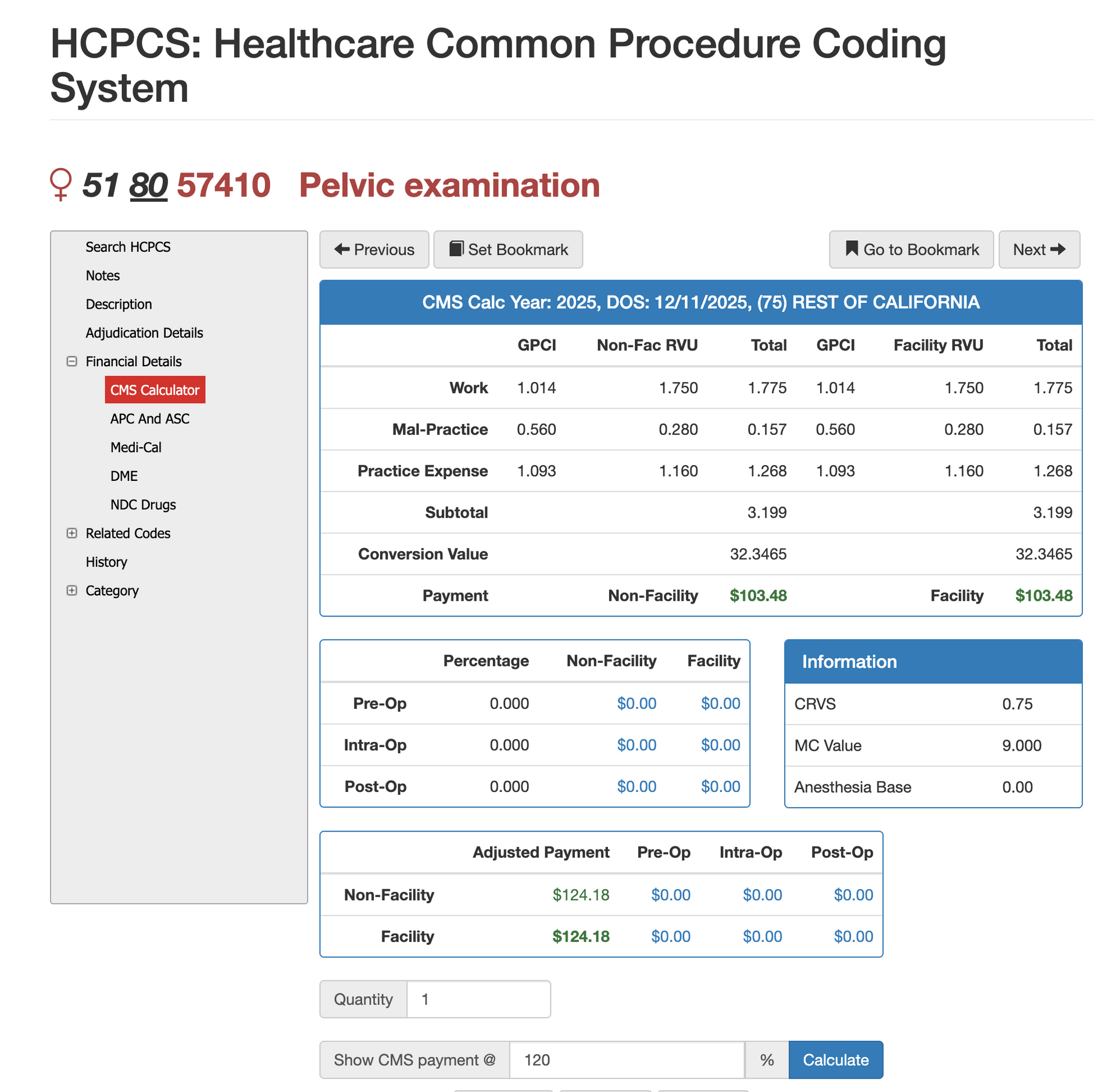
The financial value of CPT 57410 is driven by work, practice expense, and malpractice RVUs, all adjusted through the Geographic Practice Cost Index. Because this is a combined diagnostic procedure involving two distinct tissue samples, its RVU value is higher than curettage or biopsy alone. Virtual AuthTech and iVECoder allow payers and providers to model reimbursement at various Medicare percentages, compare facility and non-facility rates, and evaluate out-of-network pricing scenarios. These tools help ensure contract consistency and prevent over- or underpayment across different care settings.
The Easier Way to Research codes
For more than 30 years, PCG Software has supported Health Plans, MSOs, IPAs, TPAs, and provider organizations in improving coding accuracy, strengthening compliance, and reducing fraud, waste, and abuse. Our solutions, including Virtual Examiner®, VEWS™, and iVECoder®, are built on decades of payer-side adjudication experience and reflect the same logic used by health plans nationwide. National regulatory guidance, payer policies, compliance standards, and large-scale claims review patterns inform this CPT 69210 analysis.
Toss out the CPT book.
Stop researching articles.
Sign up for iVECoder today!
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others