CPT Code 51703 - Insert Bladder Catheter Complex
CPT Code 51703 Guide Summary
Quick Summary: CPT Code 51703 describes the complicated insertion of a bladder catheter, typically requiring enhanced skill, additional technique, or the use of specialized equipment compared to routine catheter placement. This code should not be confused with 51701 or 51702, which represent simple or non-indwelling catheter insertions. In this guide, we explain what qualifies as a “complicated” insertion, how CMS and AMA define the service, and what claims examiners look for when determining medical necessity. You’ll also see updated status indicators, documentation requirements, and visual references to help ensure accurate billing and confident claim review.
Who, What, When for CPT Code 51703
Who bills for CPT Code 51703?
CPT 51703 is primarily billed by urologists, as they most frequently perform complicated catheter insertions related to urinary retention, strictures, trauma, postoperative complications, or difficult anatomy. Emergency medicine physicians and hospitalists may also bill this code when managing acute urinary obstruction or when a routine catheter insertion becomes complex. In surgical settings, general surgeons or gynecologists may report 51703 when catheter placement requires advanced technique before or after pelvic procedures. Advanced practice providers—such as nurse practitioners and physician assistants—may bill 51703 as well, provided state scope-of-practice rules allow them to perform the procedure and payer policies support incident-to or direct billing. Across all specialties, documentation must clearly establish why the insertion was complicated to support the higher-level code.
AMA Description for 51703
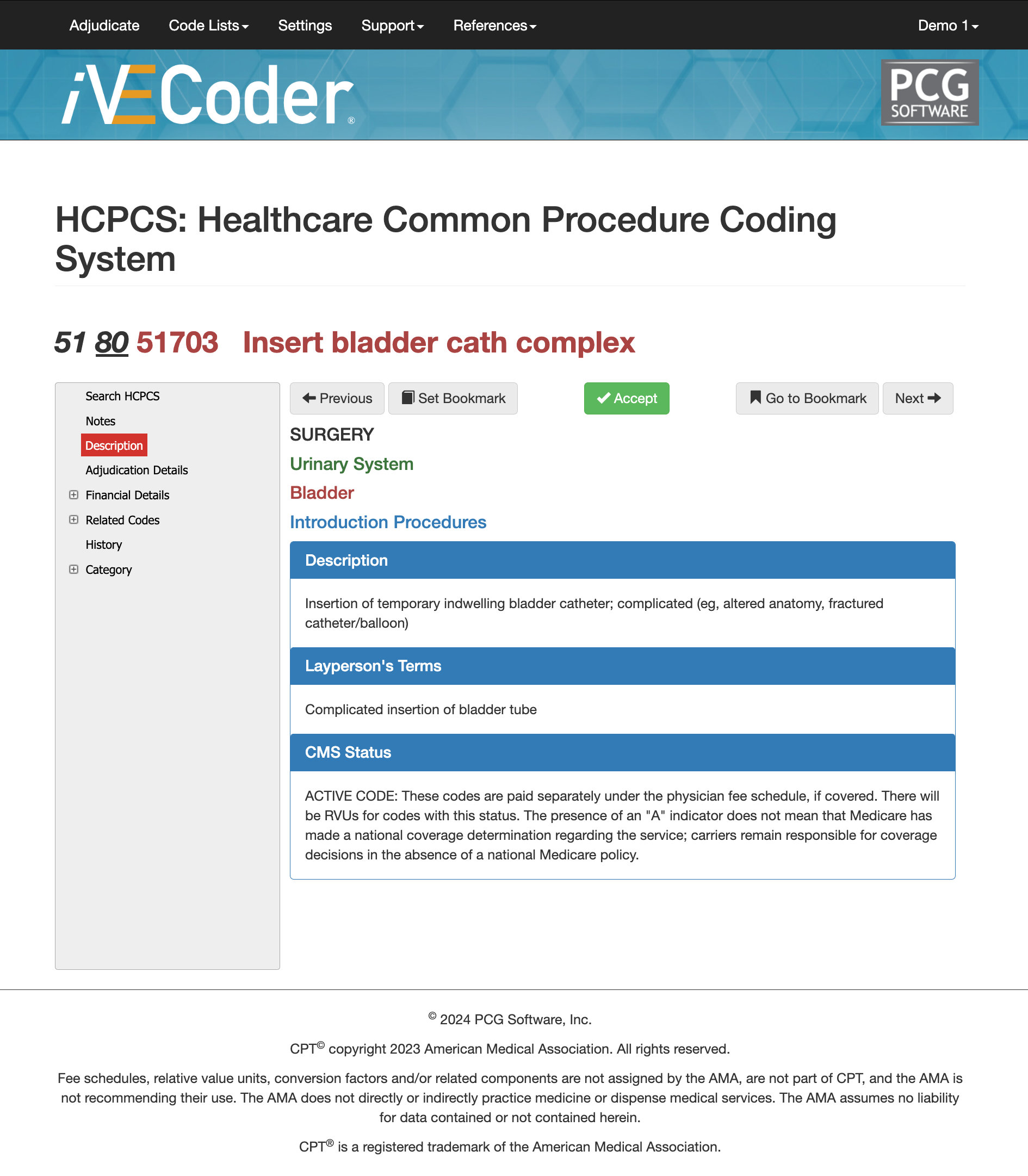
According to the AMA and CMS, CPT 51703 should only be reported if performed independently. Do not report 51701-51702 when the catheter is an inclusive component of another procedure. CPT 51701 and 51702 are paid separately under the physician fee schedule, if covered. There will be RVUs for codes with this status. The presence of an "A" indicator does not mean that Medicare has made a national coverage determination regarding the service; carriers remain responsible for coverage decisions in the absence of a national Medicare policy.
Most Common Diagnosis for CPT Code 51703
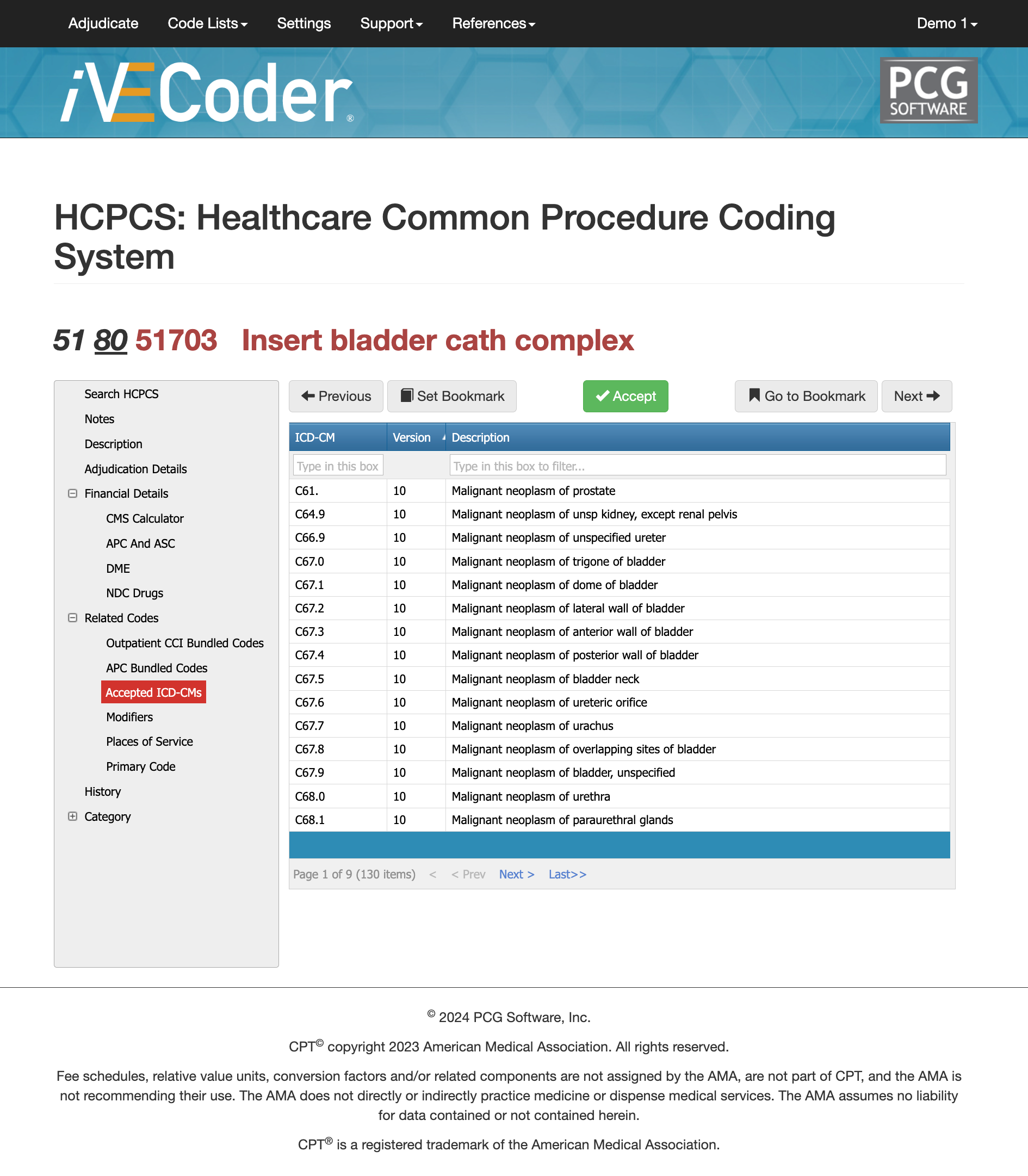
CPT 51703 is approved for a wide range of urinary tract conditions that justify a complex catheter insertion, and payers expect the diagnosis code to clearly support why the procedure was medically necessary. Common ICD-10 diagnoses include malignant obstructions of the bladder or urethra, postoperative urinary retention, strictures, traumatic injury, neurogenic bladder disorders, and other situations where a standard catheter insertion (51701–51702) would not be clinically appropriate. Diagnosis codes must reflect the specific condition causing obstruction or complexity—vague or nonspecific urinary symptoms often lead to denials or downcoding. Tools like Virtual AuthTech and iVECoder help match 51703 with the correct ICD-10 pairs and flag cases where the diagnosis does not meet payer policy or medical-necessity standards. Ensuring diagnostic alignment is one of the simplest ways to protect against avoidable claim delays or medical review.
Comparing cpt 51701, 51702, and 51703
| Code | Description | Complexity | Typical Use Case | Key Documentation Requirements |
|---|---|---|---|---|
| 51701 | Simple non-indwelling bladder catheter insertion | Low | Straight catheterization; diagnostic specimen collection; no obstructions or resistance | Note that insertion was routine, no complications, and catheter was non-indwelling |
| 51702 | Simple indwelling (Foley) catheter insertion | Low–Moderate | Routine Foley placement for retention, surgery prep, or monitoring; no abnormal anatomy or trauma | Document reason for indwelling catheter and confirmation of uncomplicated placement |
| 51703 | Complicated catheter insertion (any catheter type) | High | Urethral stricture, trauma, resistance, false passage, difficult male anatomy, postoperative swelling, prior pelvic surgery, or failed standard attempts | Clearly document the complication, attempts, techniques used, anatomical challenges, and clinical necessity for advanced catheterization |
Why Payers look at CPT 51701-57103 differently
Choosing the correct catheter-insertion code depends on the level of difficulty, the clinical context, and the documentation supporting why the procedure was routine or complicated. CPT 51701 describes the simplest scenario—temporary insertion of a non-indwelling catheter without difficulty. CPT 51702 applies when an indwelling (Foley-type) catheter is placed, still under routine conditions with no resistance or abnormal anatomy. CPT 51703, however, is reserved for complicated insertions requiring greater skill, such as when the patient has strictures, obstruction, trauma, postoperative swelling, false passages, or when standard technique fails. Claims examiners rely on differences between these codes to ensure the documentation supports why the encounter required a “complicated” insertion rather than a routine placement, as inaccurately upgrading is one of the most common reasons for denials.
Billing and Payment Tips for 51703
APC vs ASC for CPT Code 51703
51703 cpt code is part of the diagnostic family 99, has no age range, an MUE count of 2, and HOS MUE Count of 2. 51703 cpt code is part of the diagnostic family 99, has no age range, an MUE count of 2, and HOS MUE Count of 2.
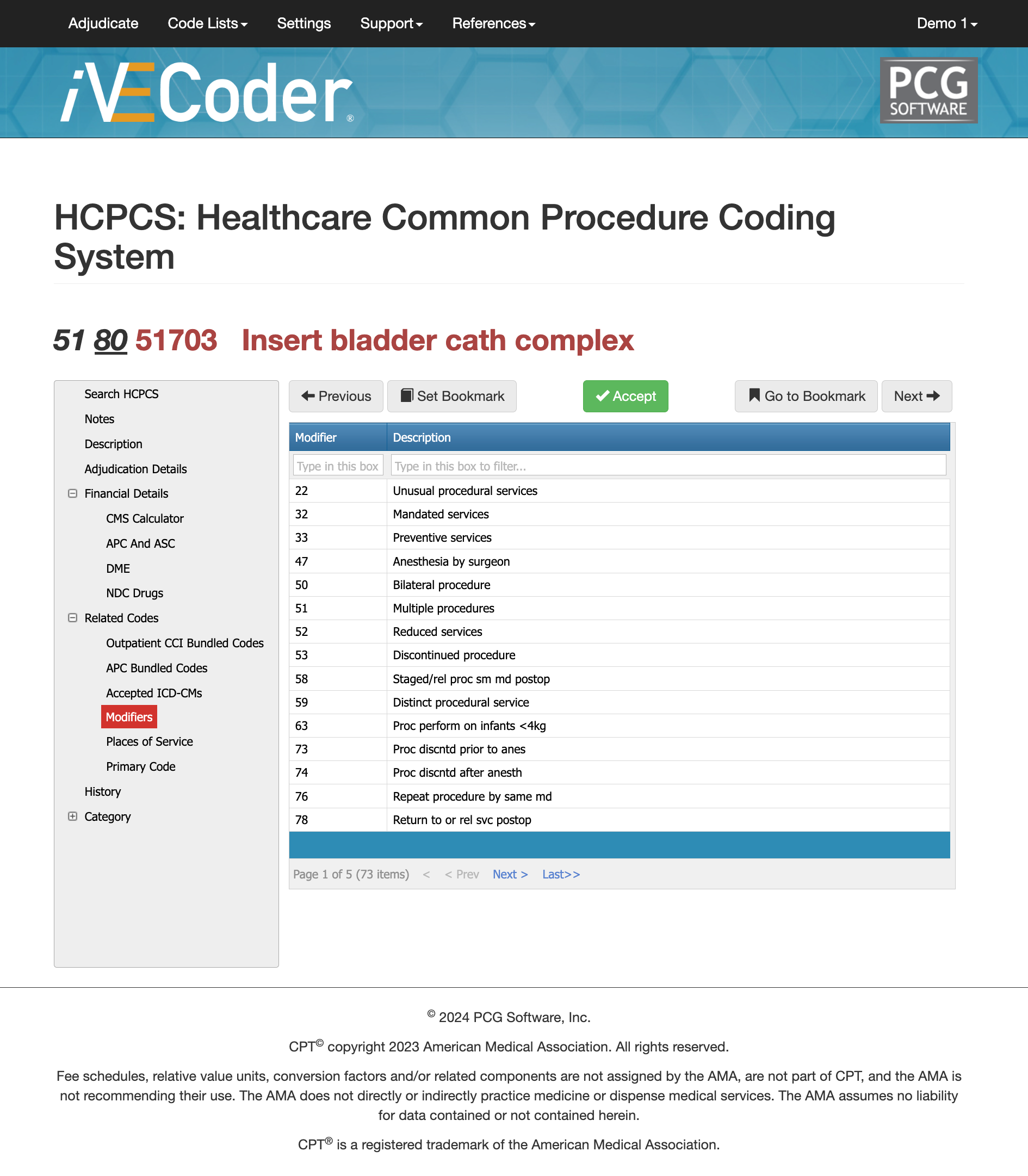
Most Commonly Used and Accepted Modifiers
Using the appropriate modifiers is crucial for ensuring accurate coding and proper reimbursement. By using iVECoder, you can run mock authorizations and adjudications with different modifiers to see the likelihood of getting a medical claim approved and learning which modifiers work best with CPT Code 51703.
Modifier 59 with CPT Code 51703
This modifier indicates that the procedure was distinct or independent from other services performed on the same day. It is used when procedures that are typically bundled together are performed in separate and distinct settings or encounters.
Modifer 25 with CPT Code 51703
Used when a significant and separately identifiable E/M service is performed by the same physician or other qualified health care professional on the same day as the procedure. This means an evaluation and management service was provided above and beyond the other service.
Modifier 51 with CPT Code 51703
Modifier 51 is used when multiple procedures are performed during the same session. It indicates that multiple services were provided and helps in the correct reimbursement of each service.
Modifier 76 with CPT Code 51703
Modifier 76 is used when the same procedure is performed more than once on the same day by the same provider. It indicates that the procedure was repeated.
Modifier 77 with CPT Code 51703
This modifier is used when the procedure is repeated by a different provider on the same day. It distinguishes the repeat procedure from the original procedure performed by another provider.
Modifier 52 with CPT Code 51703
This modifier indicates that a service or procedure was partially reduced or eliminated at the physician’s discretion. It is used when the full service described by the CPT code is not performed.
Bundled Codes for 51703 - CCI, APC, and ASC
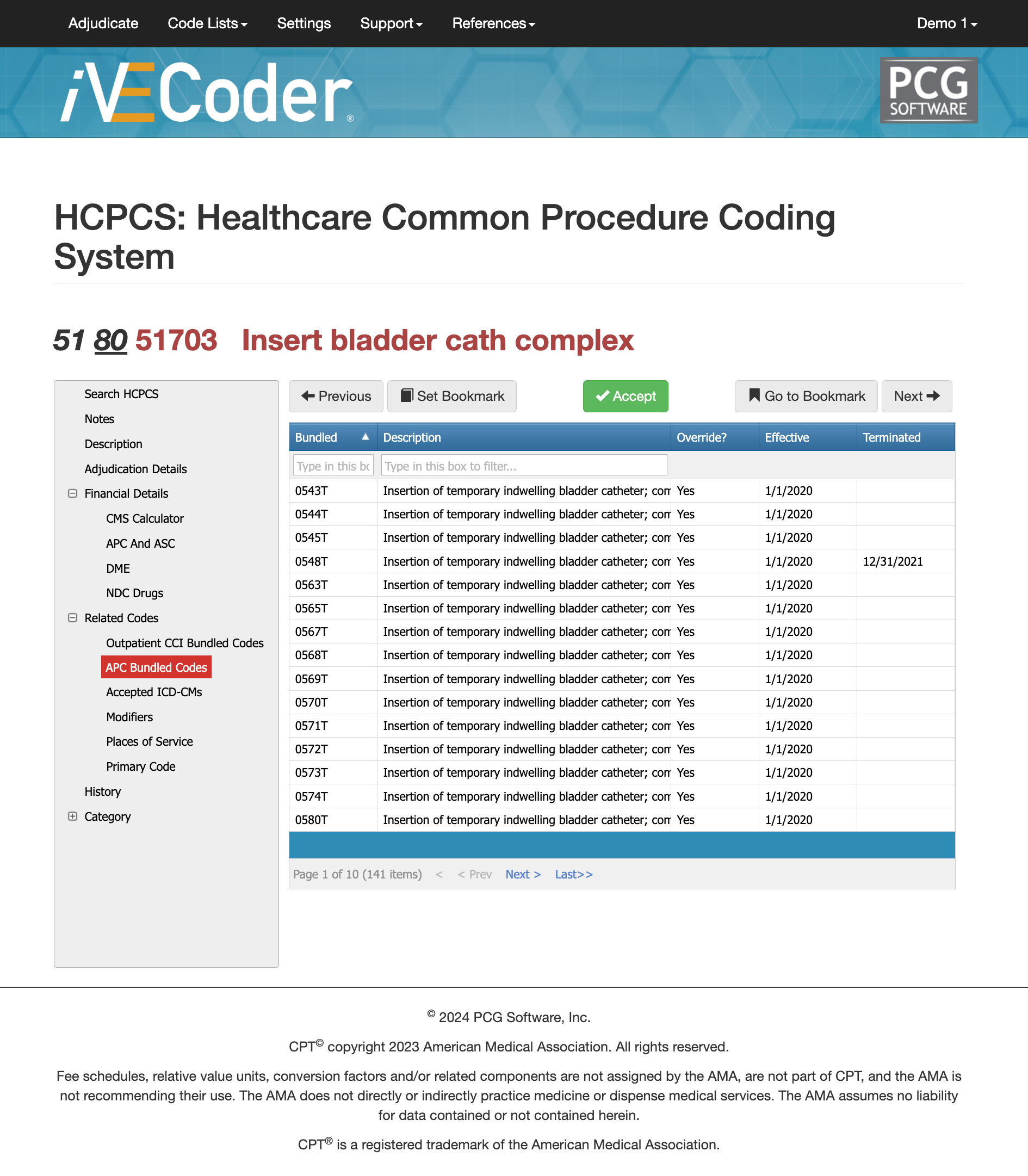
Bundling plays a major role in how CPT 51703 is paid, especially in outpatient and ambulatory surgery environments. Under the CMS Ambulatory Payment Classification (APC) system, 51703 falls under APC 05721, which covers Level I diagnostic tests and related services. Payment is based on national OPPS rates, wage-index adjustments, and facility-specific factors, meaning reimbursement varies by geographic region and wage/GEO calculations. The “S” status indicator shows that 51703 is paid separately under OPPS, but only when the service is distinct and not bundled into another primary procedure.
Across outpatient settings, CMS lists 141 possible APC bundled codes that may interact with 51703. Many of these represent other urinary catheter procedures (such as 51701 and 51702), cystoscopic services, or related diagnostic interventions. Incorrectly unbundling 51703 can result in denials, overpayments, or delayed claims that trigger post-payment audit risk. Because catheter insertion is often performed during broader urologic treatment encounters, accurate bundling depends on clear documentation and a review of CCI edits.
Software such as Virtual Examiner (payer organizations) and iVECoder (clinics and billers) helps identify bundling conflicts by scanning medical notes, reviewing modifier use, and comparing the encounter to CMS bundling logic. Using these tools before submission greatly reduces denials tied to misapplied APC codes and improves compliance for both facility and professional billing.
Stone removal bundling for 51703
Occurs when insertion is part of a larger urologic procedure, such as cystoscopy or endoscopic stone removal, and not performed as a standalone complex catheter placement.
Why ASC Payment Often Bundles 51703
ASCs frequently package catheter insertions into the primary surgical payment when CMS deems the catheter work integral to the main procedure.
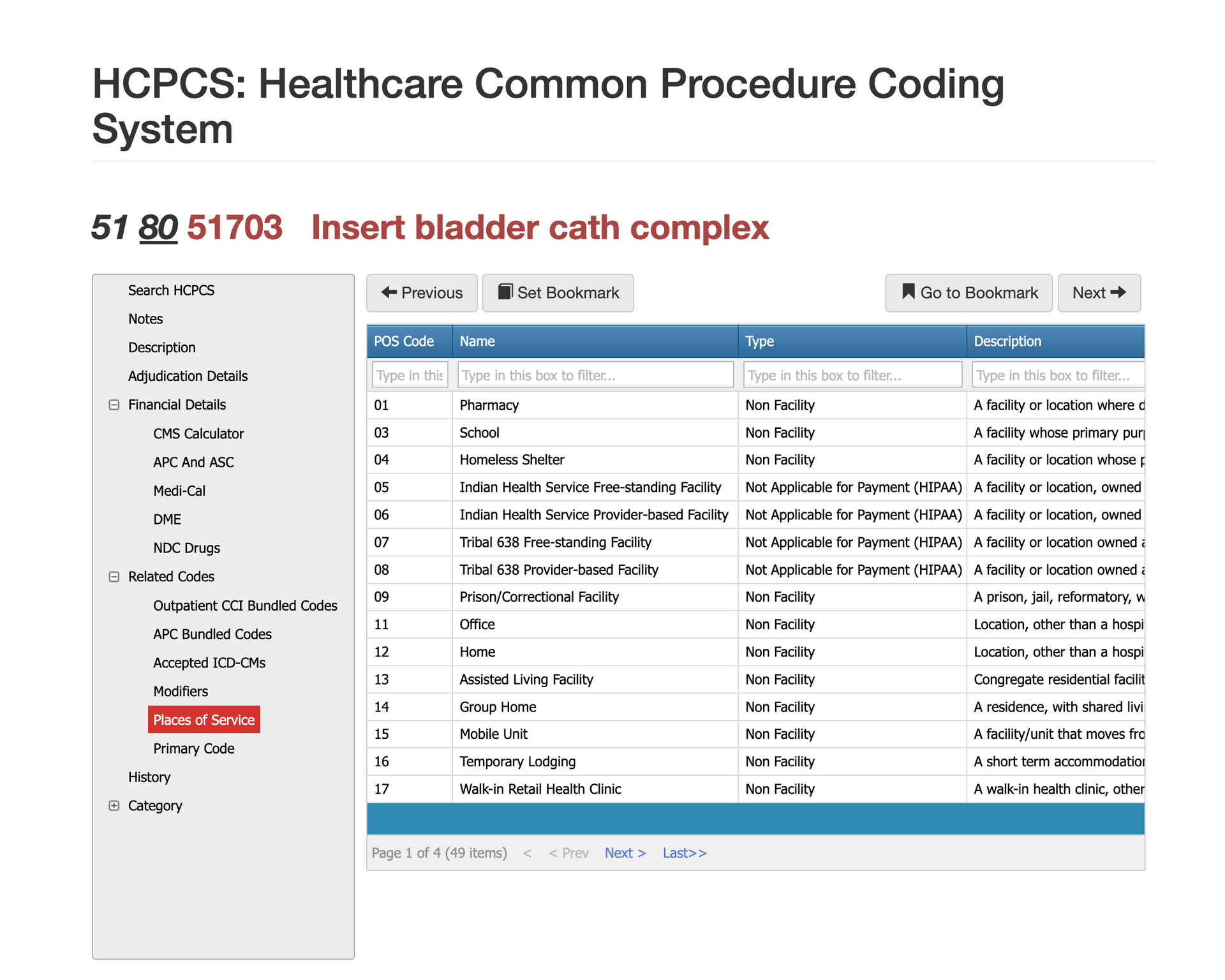
Places of Service Requirements for CPT 51703
There are more than 49 possible Places of Service (POS) codes, but only a small group is commonly associated with CPT 51703. Because this code describes a complicated bladder catheter insertion, it is most often billed in hospital outpatient departments, emergency departments, physician offices, urgent care centers, and skilled nursing facilities—settings where clinicians routinely manage difficult urinary obstructions or postoperative complications. The POS must accurately reflect where the insertion was performed, not where the patient was evaluated or triaged. Claims often deny when the POS does not align with the provider’s documentation or when the service occurs in a facility that typically bundles catheterization into its global payment. Ensuring that the POS matches the documented clinical setting helps prevent reprocessing, medical review, and downcoding.
Most Common Reasons for Denials for 51703
CPT 51703 is most often denied when documentation fails to prove that the catheter insertion was truly complex—meaning the note does not describe obstruction, false passage, stricture, postoperative anatomy, or other factors that justify using 51703 instead of 51701 or 51702. Payers also deny claims when the procedure is bundled into a larger urologic service, such as cystoscopy or endoscopic stone removal, and the provider does not explain why a separate, distinct catheter insertion was necessary. A third common denial occurs when the Place of Service or modifier does not align with the clinical scenario, particularly when billing the professional component in a facility setting. Clear documentation describing why the insertion was difficult, paired with correct POS and bundling logic, prevents the majority of 51703 denials.
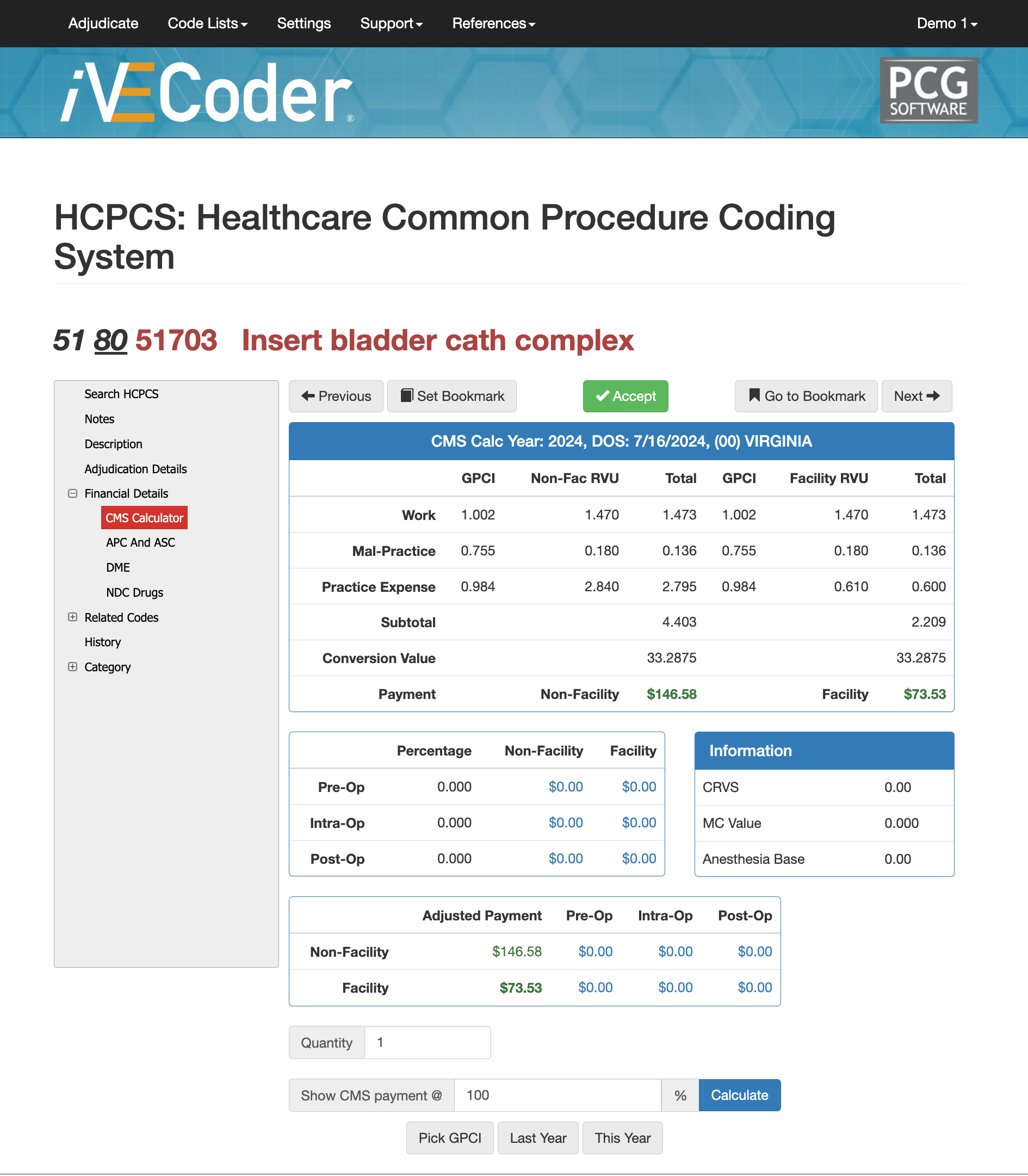
RVUS and Financials for 88323
Payment Amounts for 51703 in CMS Calculator
Reimbursement for CPT 51703 is based on its RVU components—work RVU, malpractice RVU, and practice-expense RVU—which together determine the total allowable payment under the Medicare Physician Fee Schedule. Because 51703 represents a complex catheter insertion rather than a routine placement, its RVU structure reflects the added clinical difficulty, time, and risk associated with navigating obstruction, distorted anatomy, or postoperative changes. Final payment amounts vary by geographic region through the Geographic Practice Cost Index (GPCI), meaning hospitals, ASCs, and physician offices may see different reimbursement totals based on their location and facility status.
Tools such as Virtual AuthTech (payer-side) and iVECoder (provider-side) allow users to model how reimbursement shifts when Medicare percentages, GPCI adjustments, or facility vs. non-facility values change. These tools help payers validate whether contract rates align with the complexity of 51703, while practices can evaluate out-of-network pricing and ensure accurate expected reimbursement before submitting claims. Using CMS-based percentages on a code scrubber also reduces payment disputes and supports consistent, defensible pricing across entire networks.
Comparing cpt 51703 and similar codes
| Code | Description | When It Applies | Key Difference From 51703 |
|---|---|---|---|
| 51701 | Simple bladder catheter insertion | Routine, uncomplicated placement | No obstruction or difficulty; cannot be billed when manipulation is required |
| 51702 | Straight catheter insertion, non-indwelling | Short-term, non-complex placement | Does not describe difficult or complex passage |
| 51705 | Suprapubic catheter insertion | Initial suprapubic access | Different anatomical approach; not transurethral |
| 51710 | Change of suprapubic catheter | Maintenance of existing suprapubic tract | Not comparable; catheter tract already established |
| 52000 | Cystourethroscopy (diagnostic) | Endoscopic evaluation of bladder/urethra | May occur in the same visit but follows separate CCI bundling rules |
Several catheter insertion codes sit near CPT 51703 and are commonly compared during claim review. CPT 51701 and 51702 describe simpler, non-complex catheter insertions and should not be used when the encounter requires manipulation through obstruction, false passages, stricture, or surgical reconstruction—scenarios that justify 51703. Codes such as 51705 and 51710 involve suprapubic catheter placement, while 52000 represents diagnostic cystourethroscopy, which sometimes occurs in the same encounter but follows different billing rules and bundling edits. Claims examiners review these codes together to confirm that the chosen code accurately reflects complexity and that unbundling did not occur.
Are you tired or "searching online" for CPTs?
If you’ve made it this far, you’re officially more committed than most clinicians, coders, or claims examiners—and that’s exactly why we build tools that do the heavy lifting for you. Instead of digging through long articles every time a complex CPT code shows up, iVECoder® gives both payers and providers a stand-alone scrubber that explains the rules, checks modifiers, validates documentation needs, and flags billing conflicts in seconds. And for organizations looking to go even deeper, our Virtual Examiner® (VE) claims and FWA suite identifies overpayments, detects fraud and waste patterns, strengthens compliance, and saves teams hundreds of hours each year. When you're ready to stop reading CPT blogs and start automating coding accuracy and payment integrity, we’re here to help.
Click the button right below for IVECoder or complete the form for a FREE Payer Audit.
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others