CPT 01996 defined and usage examples
What will this article about 01996 teach you?
CPT Code 01996 is used to report daily hospital or outpatient follow-up services for patients who have previously received epidural or regional anesthesia. This code captures the evaluation and management work associated with monitoring the patient’s response to the anesthetic injection, assessing pain control, managing side effects, and determining whether additional intervention is necessary. In this article, we break down the AMA and CMS definitions, documentation requirements, common denials, bundled edits, related codes, and financial considerations. You will also learn how AI code scrubbers like Virtual AuthTech and iVECoder reduce errors, ensure compliant billing, and strengthen payment accuracy for anesthesia-related encounters.
The Who, What, When for billing and paying for CPT Code 01996
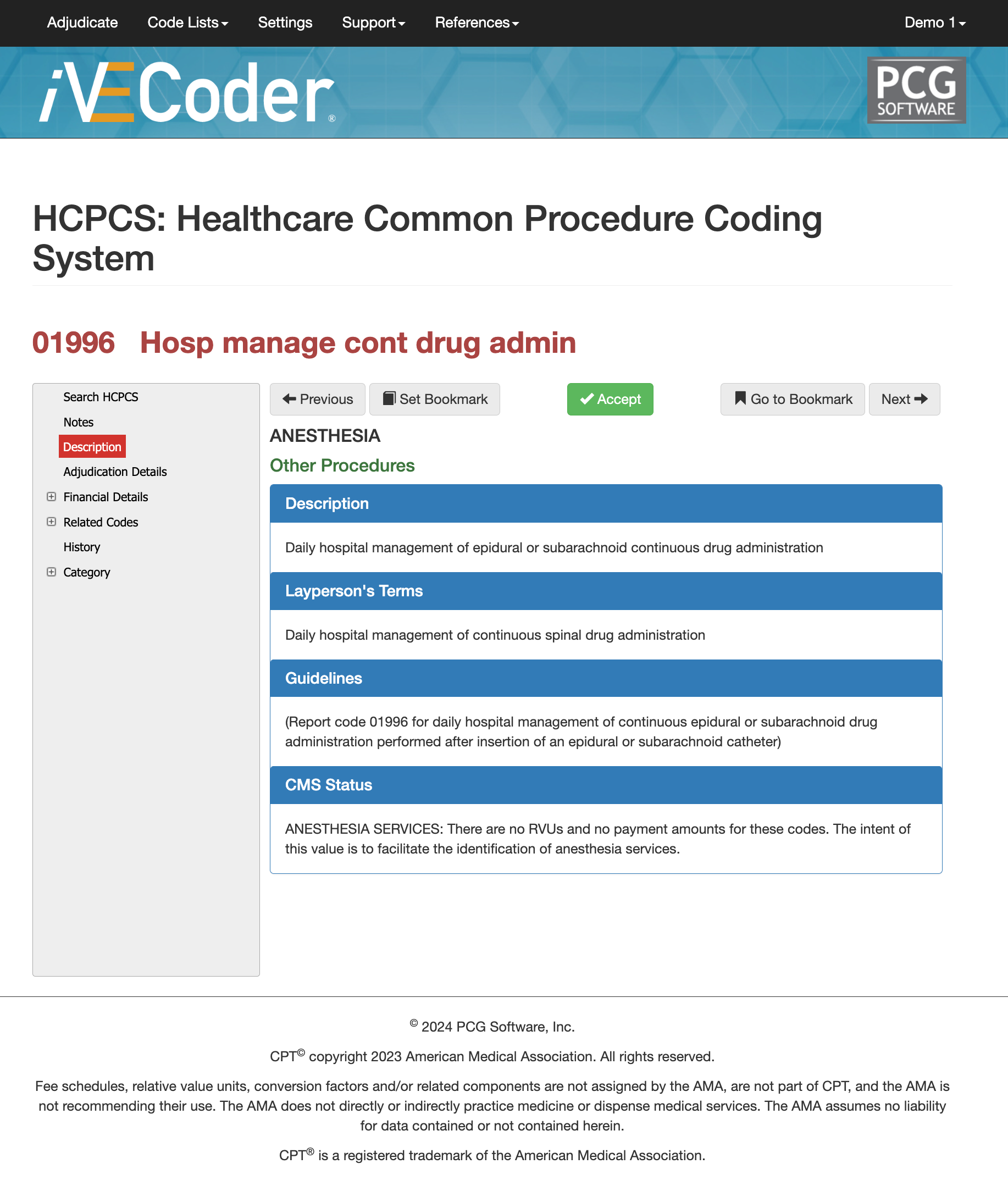
AMA Definition of CPT Code 01996:
01996 – Daily hospital management of epidural, subarachnoid, or subcutaneous continuous drug administration.
Layperson Description for CPT Code 01996:
This code is used when a provider checks on a patient after a pain-control catheter (such as an epidural catheter) has already been placed. Each day, the clinician evaluates how well the medication is working, adjusts dosing if needed, and monitors for side effects. It does
not describe placing the catheter—only the ongoing follow-up.
When is CPT Code 01996 Used?
CPT 01996 should be reported when a clinician performs daily management of an epidural or subarachnoid catheter previously inserted for pain control, typically for labor, postoperative recovery, or chronic pain management. The key requirement is that the service includes evaluation of the catheter function, assessment of analgesia, consideration of dose adjustment, examination for complications, and medical decision-making related to the catheter’s ongoing use.
This code cannot be used for initial placement, drug injection, or pump refill. It also must represent work “separate and distinct” from standard postoperative rounds or global surgical evaluation. Claims examiners frequently review these encounters to verify medical necessity—especially when 01996 appears repeatedly during a multi-day stay.
Who bills for CPT Code 01996?
CPT 01996 is most commonly billed by anesthesiologists, pain specialists, and certified registered nurse anesthetists (CRNAs) managing continuous epidural or subarachnoid infusions. In some institutions, hospitalists, obstetricians, or surgical teams may perform this service when trained to manage epidural analgesia. Advanced practice providers such as NPs and PAs may also bill 01996 when permitted under state scope-of-practice laws and payer policies. Because the code reflects medical management—not procedural work—many specialties can report it, provided their documentation shows active decision-making and catheter-specific follow-up.
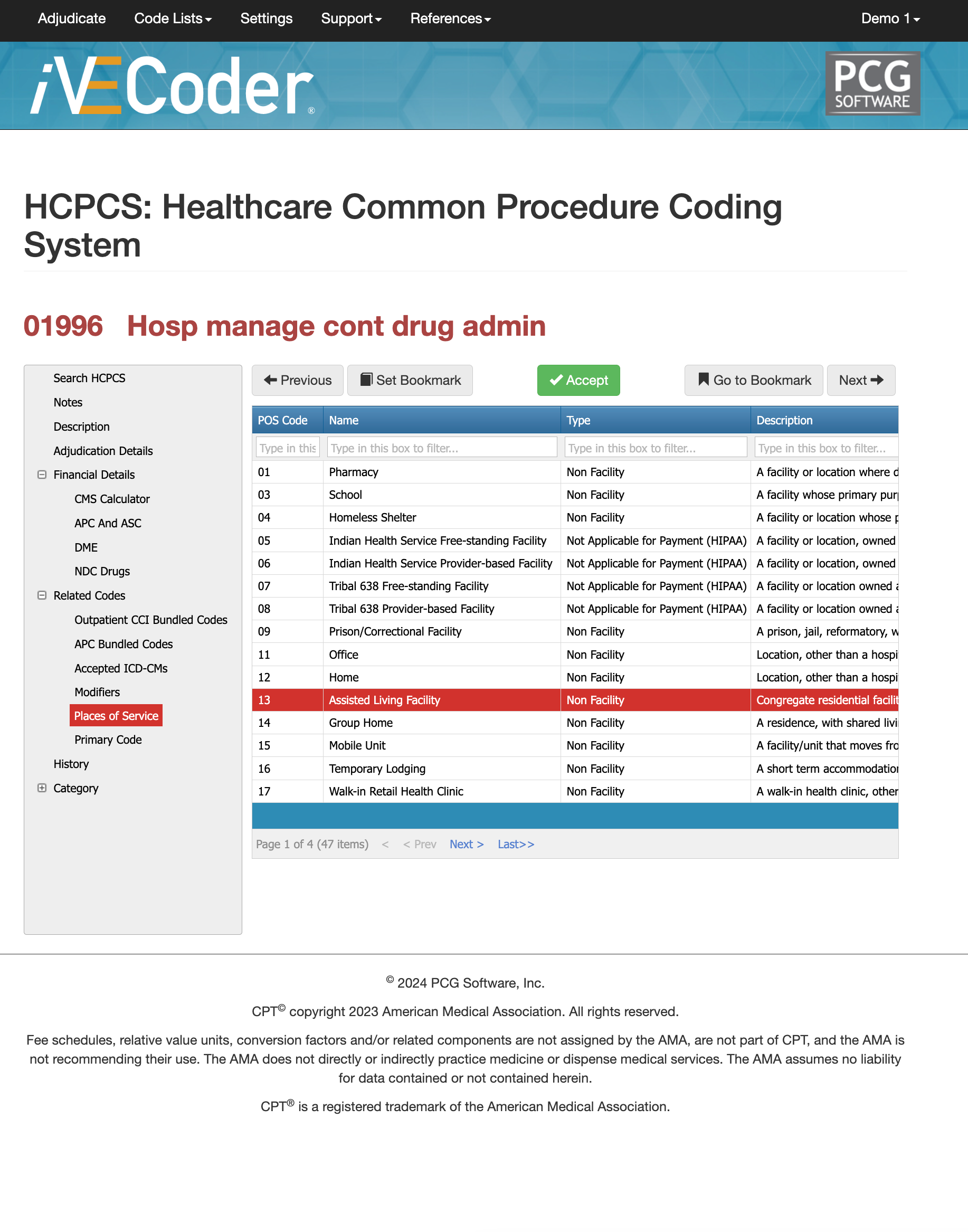
Places of Service for CPT Code 01996
Although CPT 01996 can technically be billed in multiple care settings, the most common POS locations include:
- Hospital inpatient units (POS 21)
- Hospital outpatient departments (POS 22)
- Obstetric units during labor analgesia
- Postoperative recovery floors
- Skilled nursing facilities for continuous catheter management
Payers expect the POS to match the level of clinical complexity documented. Incorrect POS coding often leads to denials or reprocessing.
Proper Documentation for CPT Code 01996
Correct billing of CPT 01996 requires documentation that reflects active management, not passive observation. Notes should include:
- Assessment of pain control or inadequate analgesia
- Evaluation of catheter function (patency, location concerns, leakage, complications)
- Monitoring for adverse effects (hypotension, motor block, urinary retention, pruritus, nausea)
- Decision-making regarding medication dose, rate, continuation, or removal
- Patient response to therapy
Payers often deny 01996 when documentation appears to be routine postoperative rounding or lacks catheter-specific medical decision-making. Clear notes describing analgesia evaluation, catheter status, and clinical reasoning significantly reduce audit risk.
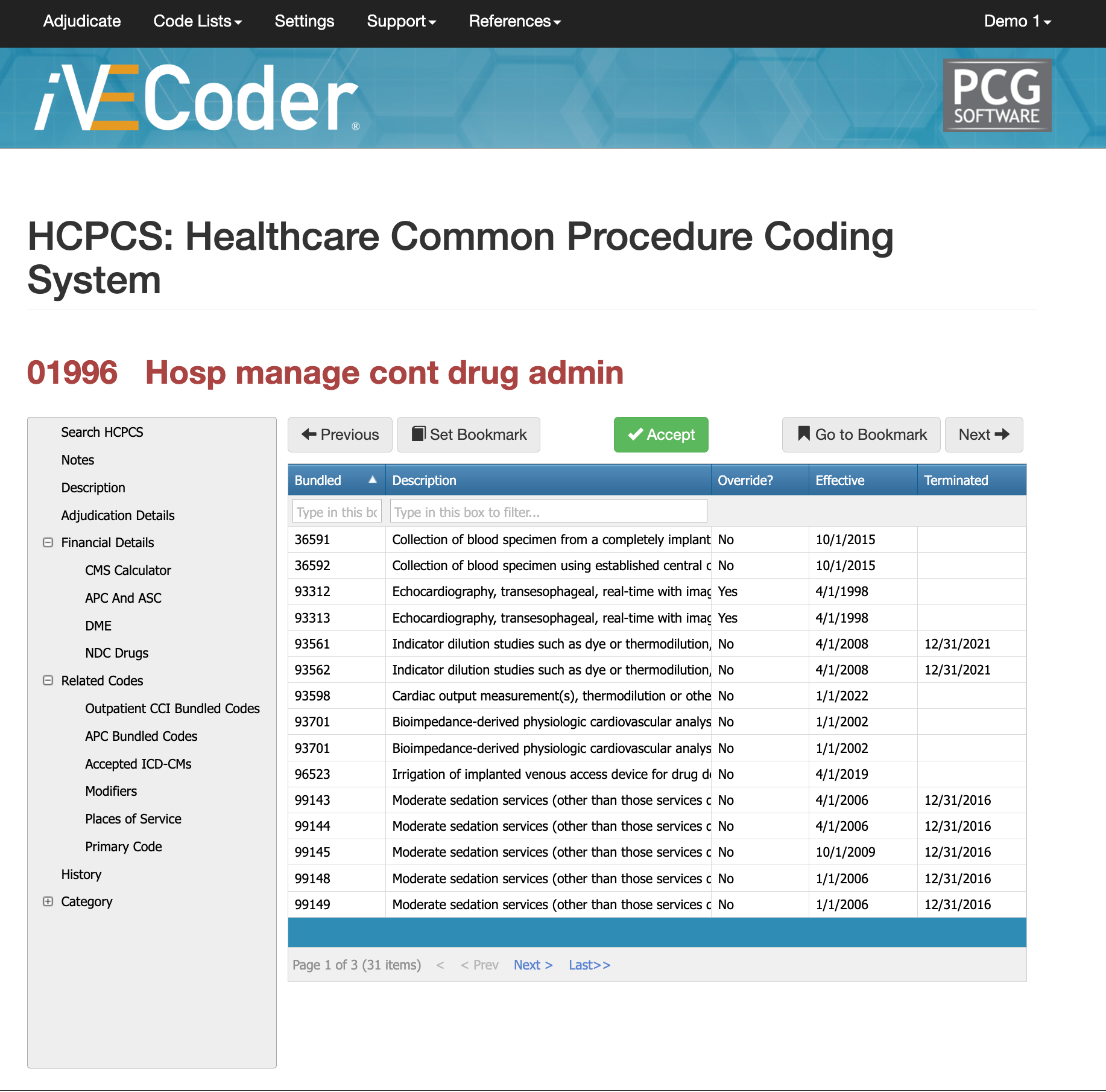
Bundled Codes for CPT Code 01996
CPT 01996 interacts with several CCI edits because certain postoperative pain-control services are bundled into surgical global periods or anesthesia-based units. The code is not separately payable when included in a global surgical package unless the management is unrelated or medically necessary beyond routine care.
Since 01996 is categorized under medical management, it generally does not receive a separate APC payment in hospital outpatient settings. In ASCs, it is typically packaged into the primary surgical service. Claims are often denied when 01996 is unbundled without justification, or when the global period of another procedure overlaps with the date of service.
Virtual Examiner and
iVECoder can help detect bundling conflicts by comparing billed codes, modifiers, and clinical notes before submission, preventing incorrect unbundling and financial loss.
Related CPT Codes for 01996
CPT 01996 sits within a small family of anesthesia and pain-management codes that distinguish between
initial catheter placement,
single-shot injections, and
daily follow-up management. Understanding how these adjacent codes differ helps claims examiners verify that 01996 is being used only for ongoing catheter oversight—not for procedural work or initial analgesic administration. The table below highlights the most commonly compared codes and how they differ from 01996.
| Code | Description | When Used | Key Difference |
|---|---|---|---|
| 1990 | Anesthesia for procedures on nerves/plexus | Simple regional anesthesia | Does not include daily management |
| 1991 | Anesthesia for procedures on nerves/plexus | More complex regional blocks | Still not daily follow-up |
| 1992 | Injection of anesthetic agent into spinal canal | Single-shot injection | No catheter management |
| 62326 / 62327 | Epidural catheter placement | Initial procedure | Not daily management |
| 1996 | Daily epidural/subarachnoid catheter management | Day-to-day evaluation & adjustments | Follow-up work only |
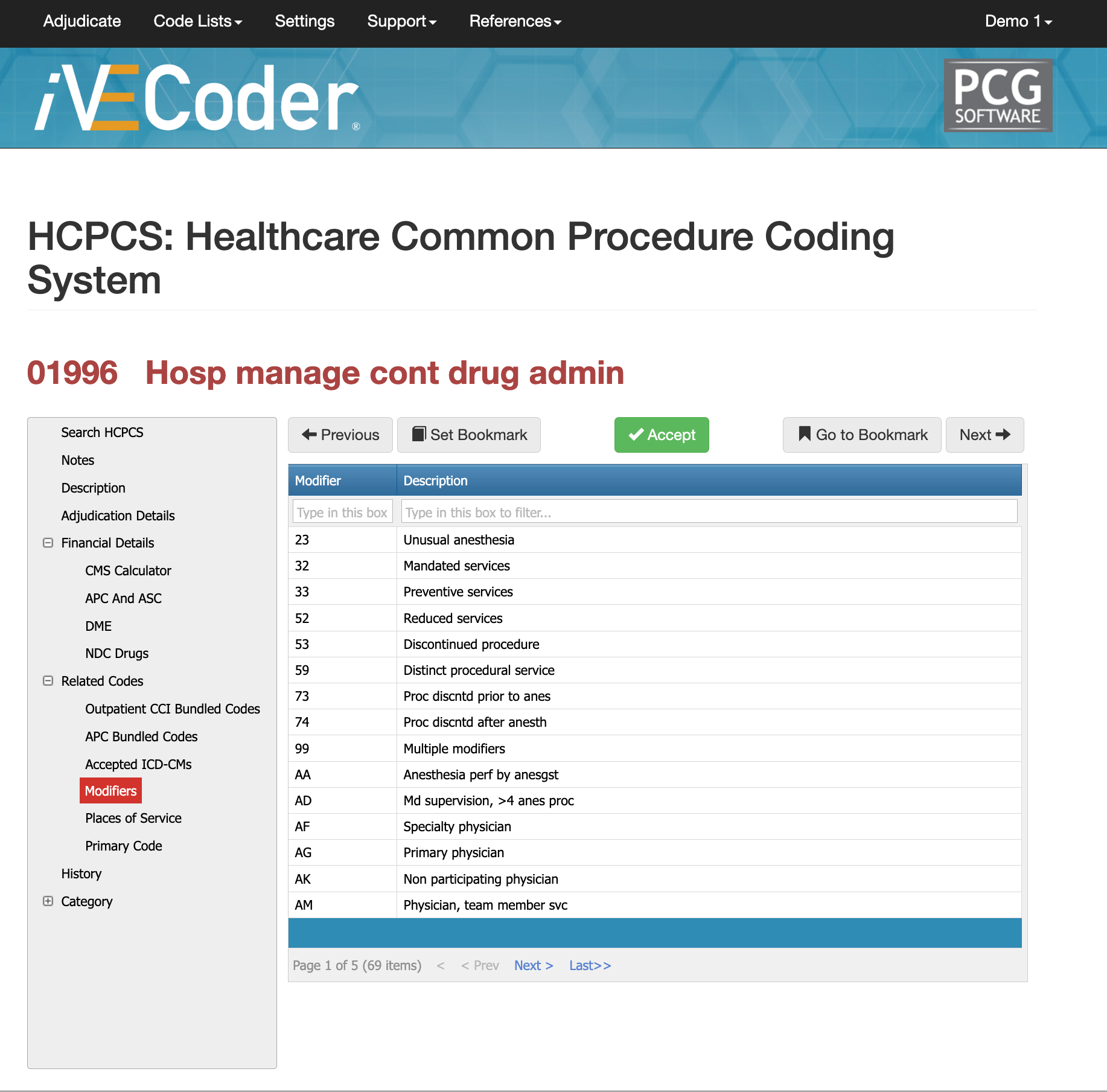
Modifier Guidance for CPT Code 01996
Modifier use for CPT 01996 is highly scenario-dependent because this code describes daily management of an epidural or subarachnoid catheter, not a procedure. Most denials occur when modifiers are applied incorrectly—especially in global surgical periods or hospital settings. Only a few modifiers are routinely accepted for 01996, and each must be supported by documentation showing why the service is distinct from standard postoperative care. Incorrect modifier use can cause automatic bundling, downcoding, or complete claim rejection, so payers typically examine these claims closely.
Modifier 24 for CPT Code 01996
Modifier 24 may be used when catheter management is performed during a global surgical period but is unrelated to the surgery being followed. For example, if an epidural catheter was placed for labor analgesia but the patient has a separate surgical recovery underway, 01996 may be billable with modifier 24 if documentation clearly distinguishes the service. Without explicit justification, payers generally bundle 01996 into the global package.
Modifier 25 for CPT Code 01996
Modifier 25 applies when a provider performs an E/M service on the same day as daily catheter management and the two services are distinct. The E/M portion must include additional evaluation, decision-making, or management unrelated to the catheter. Routine postoperative rounding, brief pain checks, or exam elements already captured in 01996 do not support modifier 25.
Modifier 59 for CPT Code 01996
Modifier 59 is rarely used with 01996 but may apply when the catheter management is clearly separate from another billed service on the same day. Documentation must support that the catheter review involved unique decision-making and was not integral to another procedure or evaluation. Because misuse of modifier 59 is a common audit finding, payers scrutinize these claims heavily.
Most Common Reasons for 01996 CPT Denials
The top denials for CPT 01996 include:
- Documentation not showing active catheter management (examiners see “routine follow-up” instead of medical decision-making).
- Bundling into global surgical packages, especially for postoperative pain control, unless modifier 24 or other justification applies.
- Diagnosis mismatch, where the ICD-10 code does not clearly support continued monitoring or analgesic adjustment.
Clear, catheter-specific notes remain the single best defense against denials.
The Easier Way to Research codes
For more than 30 years, PCG Software has supported Health Plans, MSOs, IPAs, TPAs, and provider organizations in improving coding accuracy, strengthening compliance, and reducing fraud, waste, and abuse. Our solutions, including Virtual Examiner®, VEWS™, and iVECoder®, are built on decades of payer-side adjudication experience and reflect the same logic used by health plans nationwide. National regulatory guidance, payer policies, compliance standards, and large-scale claims review patterns inform this CPT 69210 analysis.
Toss out the CPT book.
Stop researching articles.
Sign up for iVECoder today!
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others