CPT Code 20160 Defined and Usage Explained
CPT Code 20160 Sumary
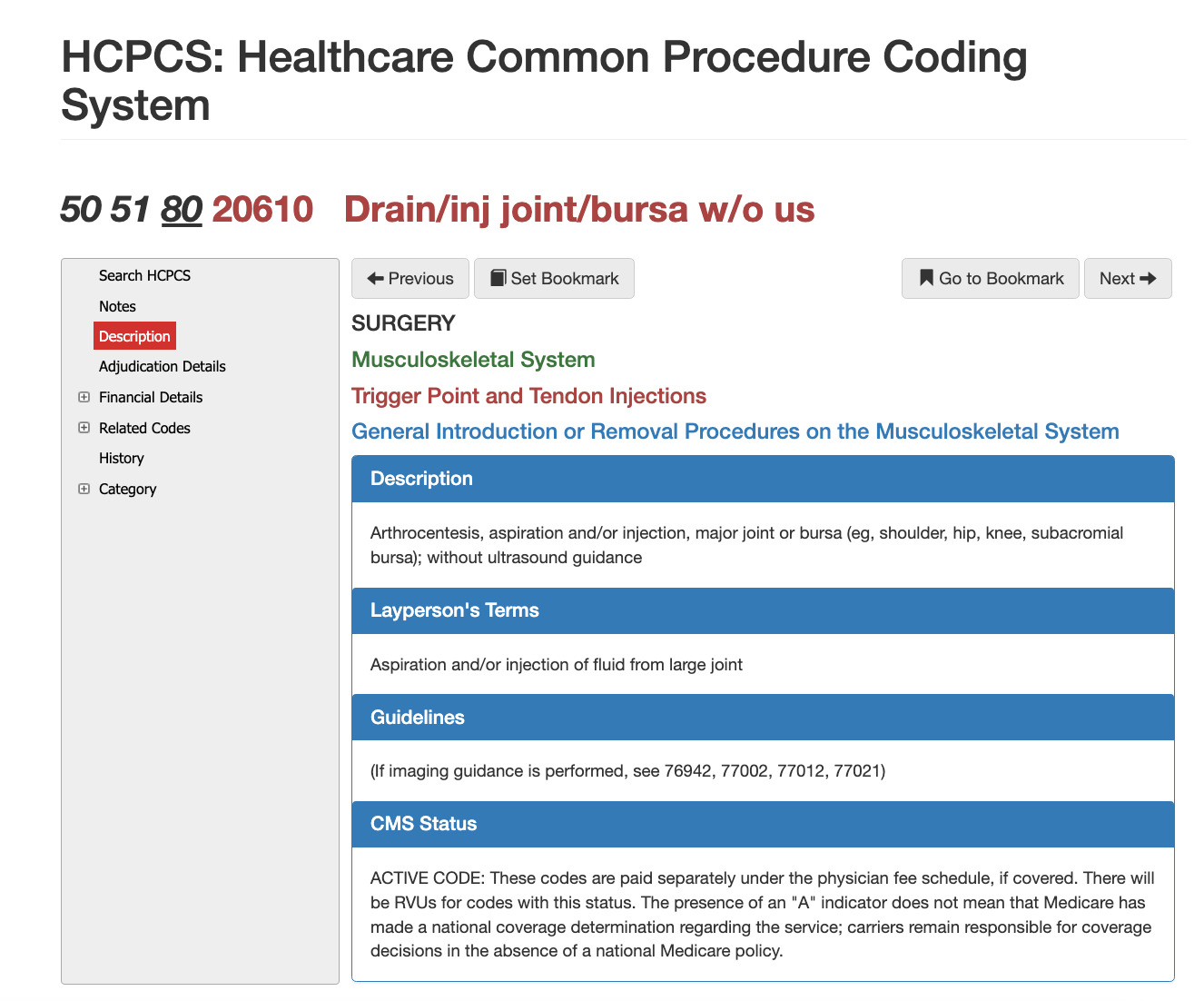
CPT code 20610 refers to procedures involving the aspiration and/or injection of fluid from major joints or bursae, such as the shoulder, hip, knee, or subacromial bursa, without the use of ultrasound guidance. This procedure is often used to treat conditions like joint inflammation or fluid buildup. If imaging guidance (such as ultrasound or fluoroscopy) is used, separate CPT codes may apply. This code is active under the Medicare Physician Fee Schedule and is reimbursed separately if covered, although local Medicare carriers are responsible for making coverage determinations in the absence of a national policy.
20160 CPT AMA Definitions below:
AMA definition: Arthrocentesis, aspiration and/or injection, major joint or bursa (eg, shoulder, hip, knee, subacromial bursa); without ultrasound guidance.
Layperson:
- Aspiration and/or injection of fluid from large joint.
- May be coded as 20610 Drain/inj join/burse w/o us (50, 51, 80)
What and when do you use cpt code 20160
What Providers bill 20610 the most?
A wide variety of clinicians bill CPT 20610, including orthopedic surgeons, sports medicine physicians, rheumatologists, pain specialists, primary care physicians, physiatrists, and emergency medicine providers. Nurse practitioners and physician assistants may also perform and bill 20610 when permitted under state scope of practice and payer rules. Because this is one of the most common musculoskeletal procedures, commercial payers, Medicare, and Medicaid all reimburse it routinely when documentation supports the diagnosis and necessity.
Proper Documentation for getting 20610 Approved
To support CPT 20610, the medical record must specify the
joint treated, the
indication (such as effusion, arthritis, bursitis, synovitis, or pain), whether
aspiration,
injection, or
both were performed, and the materials used, such as corticosteroids, anesthetics, or viscosupplement agents. Documentation should also include the technique, patient response, and any imaging guidance used. Missing details—such as failing to identify the joint or omitting the type of medication injected—are among the most common causes of payer denials.
When 20610 May be Reported with an E/M Code
Providers may report an E/M service on the same day as 20610 when a
significant and separately identifiable evaluation is performed beyond the decision to perform the procedure. This typically occurs during a new complaint evaluation or when medical decision-making is complex. To bill both, documentation must demonstrate the standalone nature of the E/M visit, and modifier
25 must be appended to the E/M code. The procedural note for 20610 does not count toward E/M documentation.
Crisis or Emergency scenarios for 20610
CPT 20610 is not used for emergent stabilization or trauma care. When joint aspiration is performed as part of emergency management—such as suspected septic arthritis or hemarthrosis—the procedure is still billed as 20610, but the visit itself may be classified under emergency department E/M codes. The presence of infection, trauma, or acute effusion does not change the CPT code but requires more detailed documentation to support medical necessity.
Adjudication Details for CPT 20610
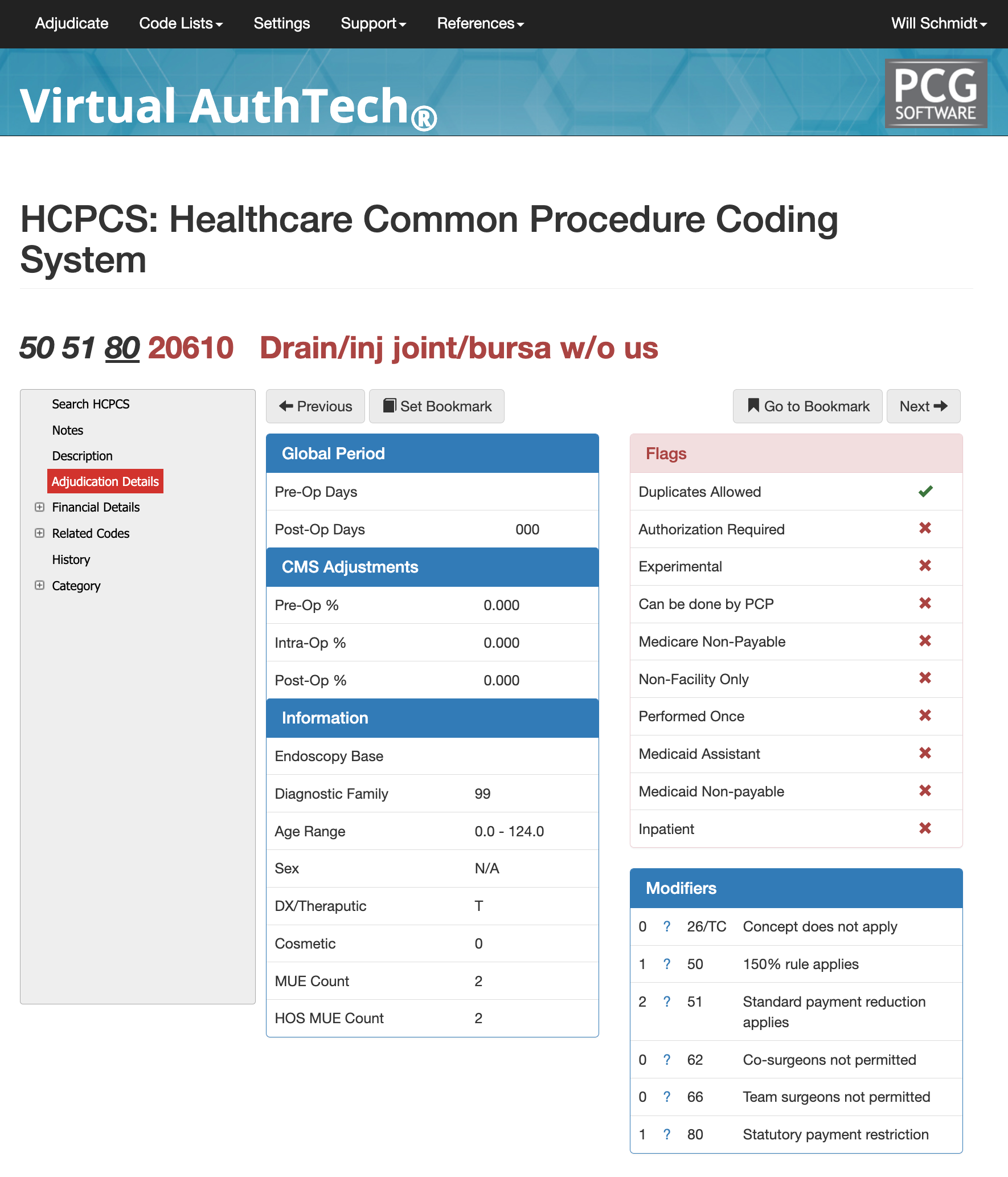
Adjudication Details for CPT Code 20610
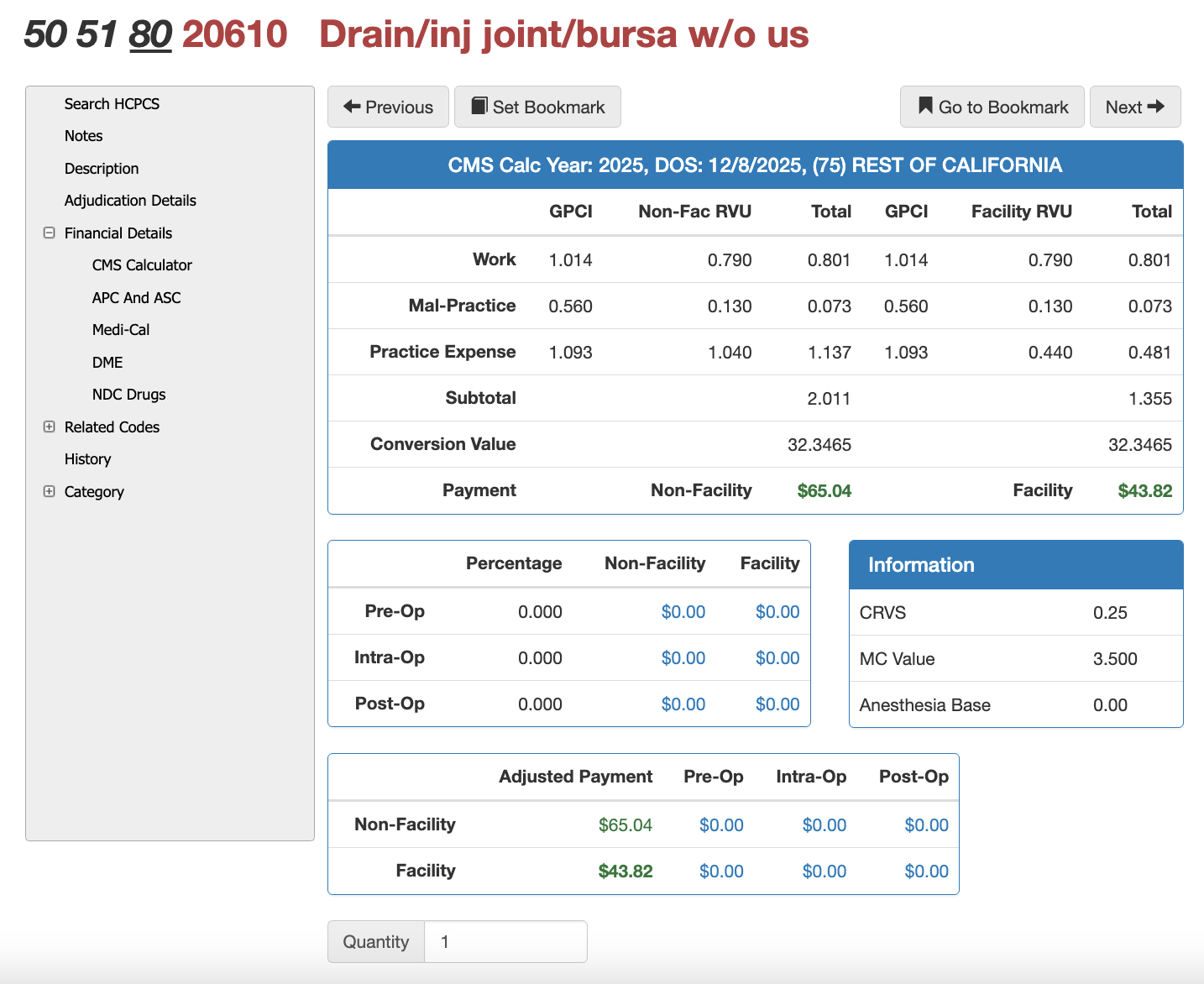
The picture below illustrates VA's findings for CPT Code 20610 against APC, ASC, and California Medicaid (Medi-Cal). You would want to set your GPCI and state medicaid settings for your own company location.
APC for 20610
- Group 05441
- Level 1 Nerve Injections
- Payment Weight: 3.22950
- Status Indicator: %
- Payment Indicator: 1
- 60%/40% Labor Split: $169.32 / $112.88
- Wage / GEo Adjustment: $257.18
ASC for 20610
- Payment Indicator: P3
- Description: Drain/inj joint/bursa w/o us
- Payment $34.61
- Wage/Geo Adjustment $26.26 (1.2645)
- Wage Adjusted Total $39.19
- Member Copay @ 20%: $7.84
- Final ASC Payment: $31.35
In hospital outpatient settings, 90837 falls within Level 3 Health and Behavior Services, making it subject to bundling under the applicable APC group. Under the ASC payment system, 90837 is not separately reimbursable and is typically packaged as part of the broader encounter. State Medicaid programs vary widely in their reimbursement for 90837, with some requiring prior authorization or imposing strict frequency limits. Providers should verify state-specific rules through Medicaid fee schedules or adjudication modeling tools like Virtual AuthTech.
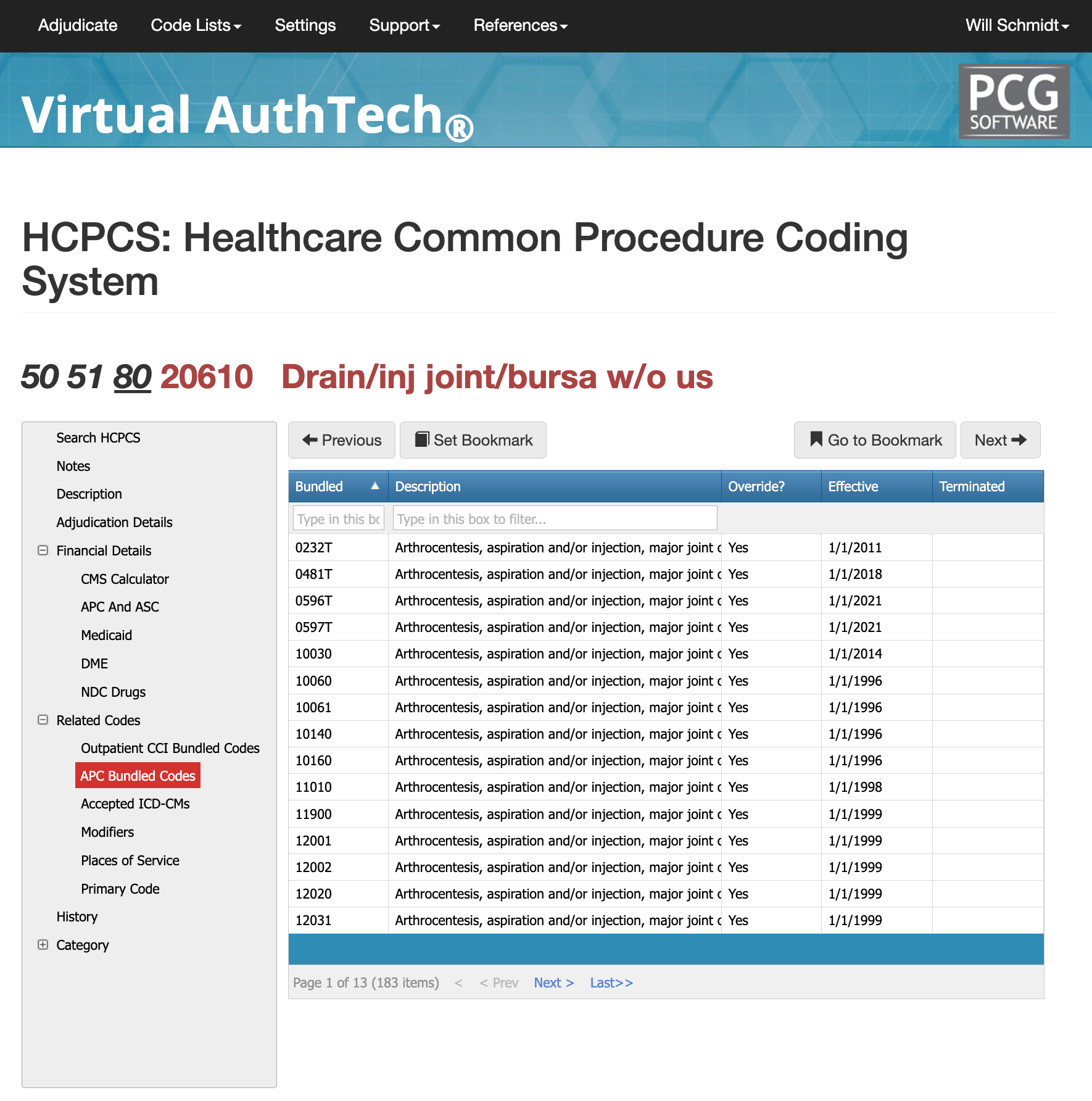
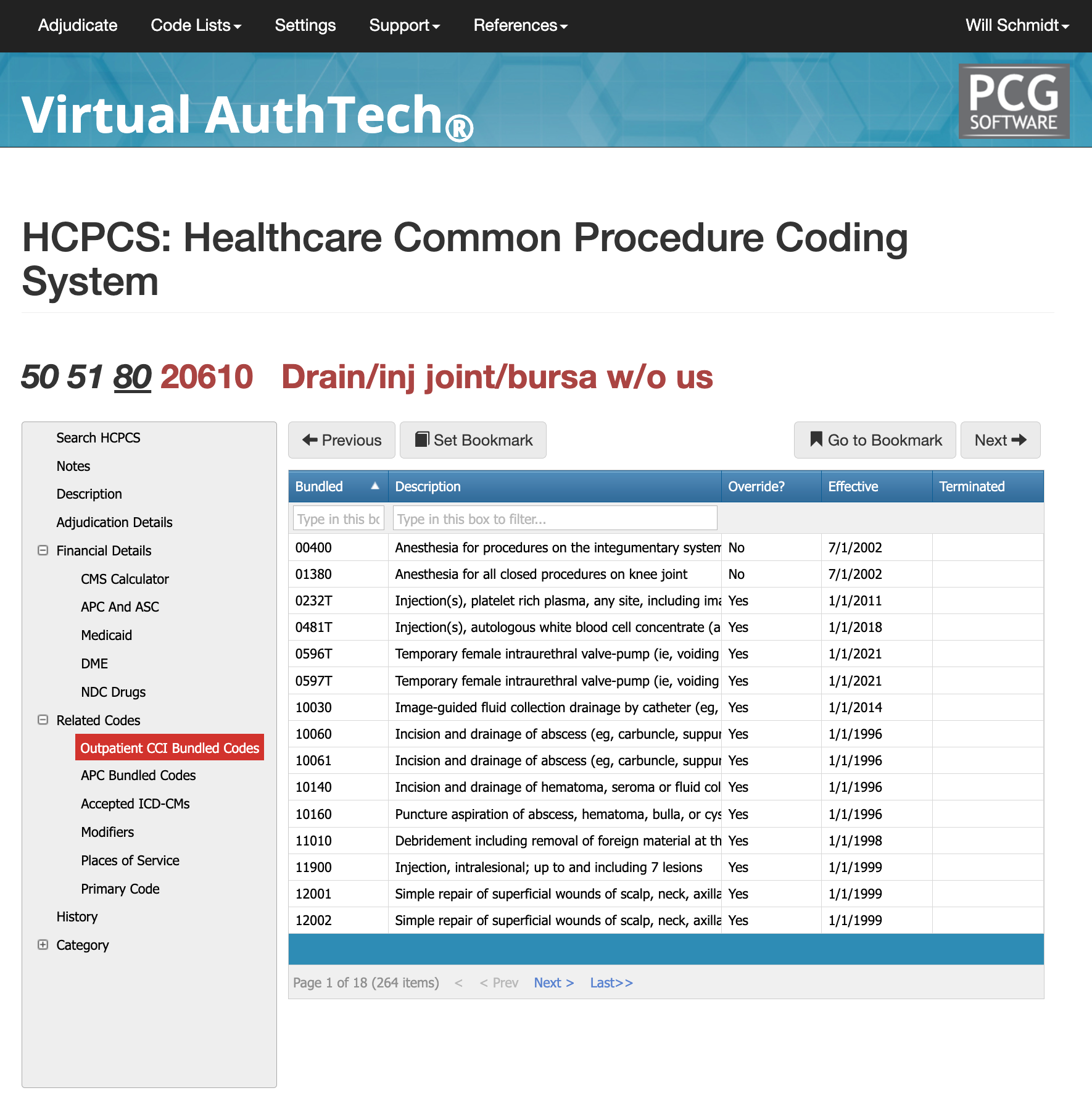
CCI Bundling and Commond Edit Conflicts with CPT Code 90837
There are 264 outpatient CCI bundled codes associated with CPT 20610, along with 183 APC bundled codes and 263 potentially related ICD-10 diagnosis pairings. Because arthrocentesis interacts with a wide clinical range of musculoskeletal and rheumatologic conditions, proper bundling review is essential to ensure compliance. Before submitting a claim, providers and payers should evaluate the procedure, associated diagnoses, imaging guidance, and any additional procedures performed on the same day. Using a claims adjudication tool such as Virtual AuthTech enables both provider and payer organizations to verify whether 20610 is separately reportable, bundled into another service, or subject to modifier requirements.
Places of Service for CPT Code 20610
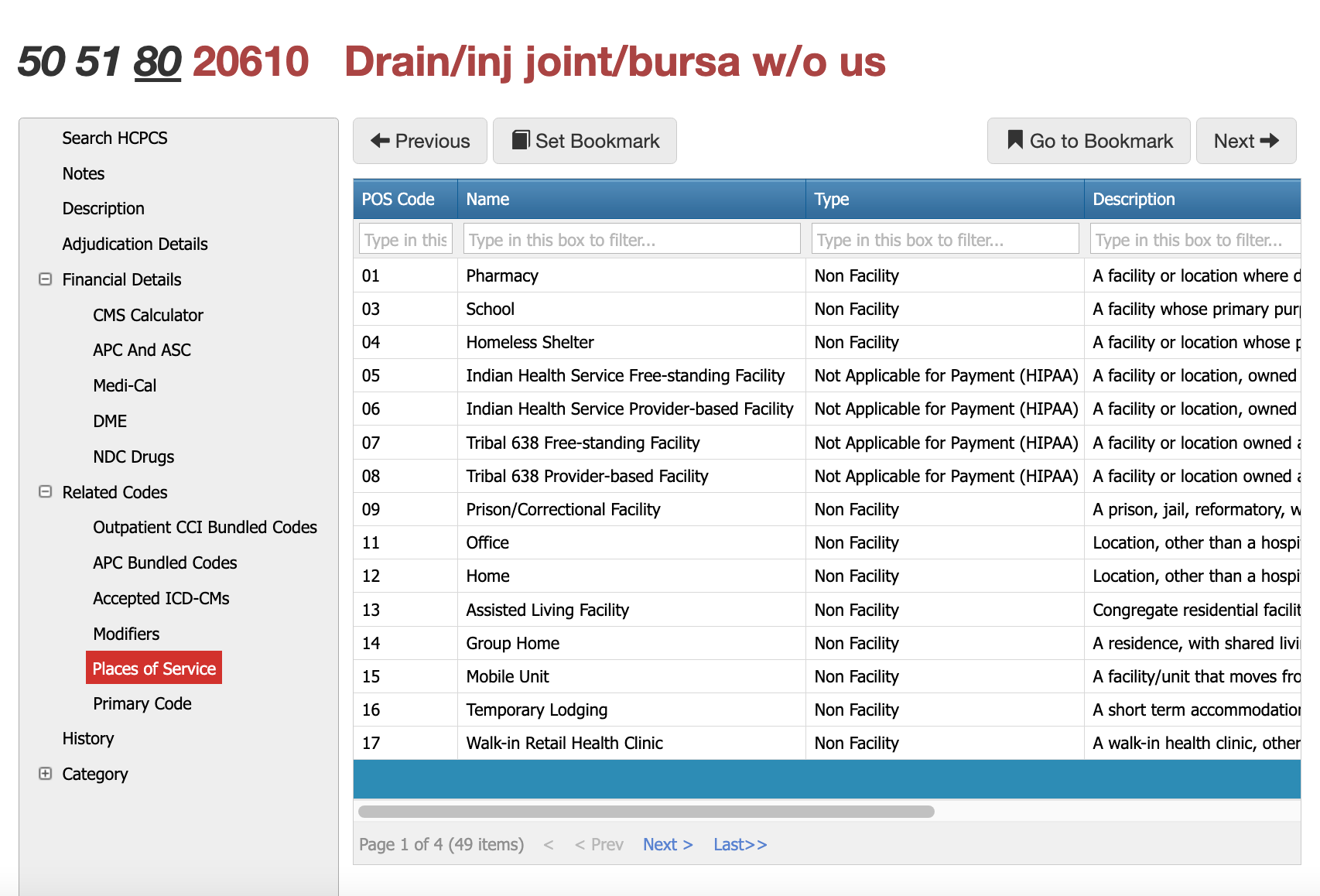
CPT 20610 is performed across a broad spectrum of clinical settings. The most common place of service is the physician office (POS 11), where joint injections and aspirations are typically performed for pain, effusion, bursitis, or arthritis management. The procedure is also routinely performed in outpatient hospital clinics (POS 22 or 19), ambulatory surgery centers (POS 24) when imaging guidance or sterile technique is required, and emergency departments (POS 23) when aspiration is medically necessary to rule out infection or manage acute swelling. Skilled nursing facilities (POS 31) and home-based care (POS 12) may also report 20610 when permitted by payer policy and scope-of-practice rules. Documentation must align with the place-of-service code reported and reflect clinical necessity for performing arthrocentesis in that setting.
Most commonly used modifiers for 20610 CPT
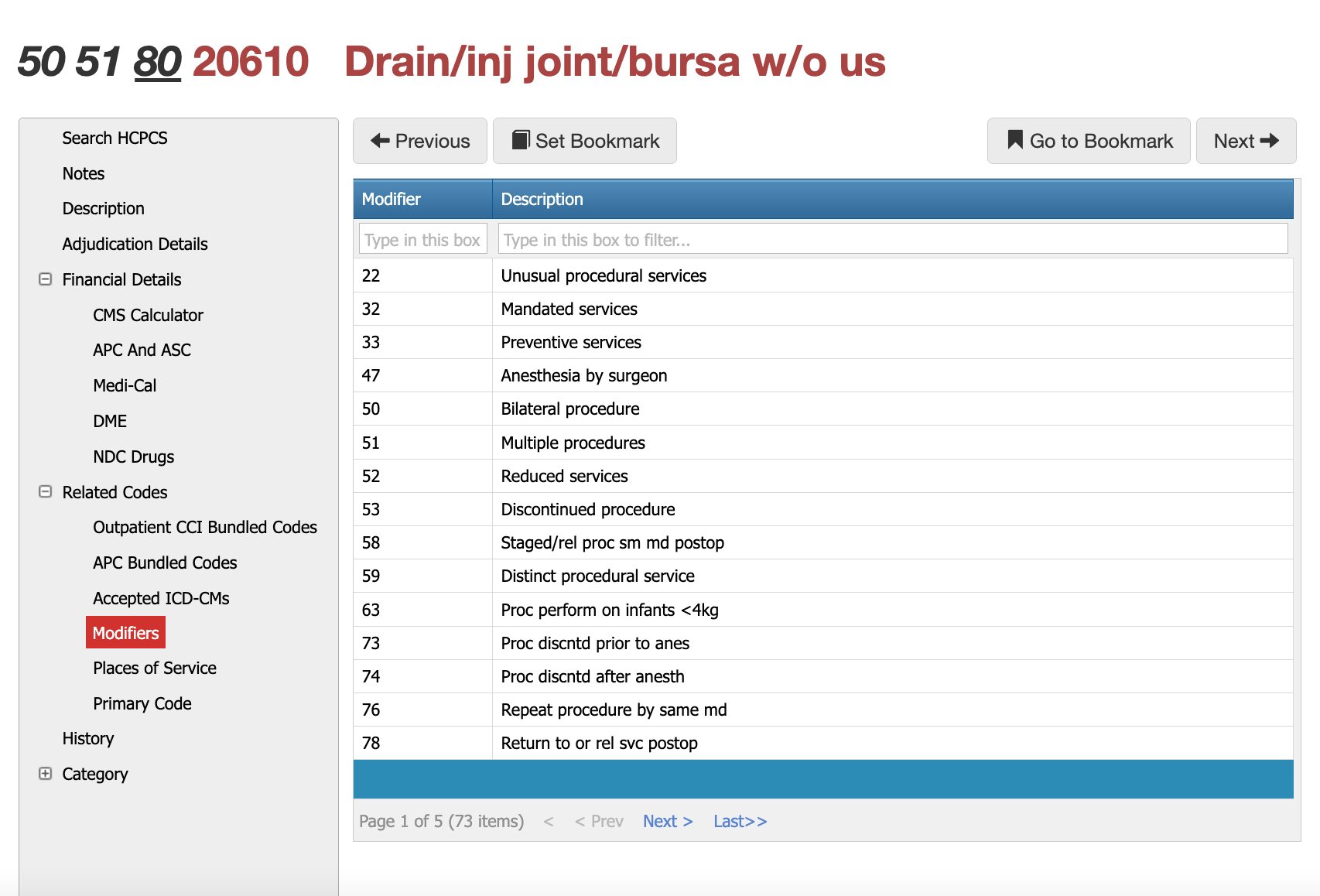
Modifier 50 — Bilateral Procedure
Modifier 50 applies when the procedure is performed on both joints or bursae during the same session. For example, if a patient receives injections in both knees or both shoulders on the same date of service, CPT 20610 would be billed with modifier 50 to indicate bilateral work. Many payers increase reimbursement for bilateral procedures, while others adjust payment based on bilateral reduction rules or local carrier policies. Documentation must specify both anatomical sites and confirm that clinically necessary treatment was performed on each side.
Modifier 51 — Multiple Procedures
Modifier 51 is used when 20610 is performed alongside other procedures in the same encounter. For instance, a clinician may inject a knee using 20610 and also perform a separate procedure on the shoulder requiring a different CPT code. In these cases, modifier 51 is appended to the secondary procedure(s) to signal multiple services. Reimbursement is typically reduced for the subsequent procedures according to payer-specific multiple-procedure fee schedules. Before billing modifier 51, clinicians should confirm whether NCCI bundling edits allow separate reimbursement.
Modifier 59 — Distinct Procedural Service
Modifier 59 remains one of the most scrutinized modifiers for joint injections. It is used when 20610 is performed on a distinct anatomical site or involves a separate and independent procedural service from another performed the same day. Modifier 59 is only appropriate when documentation clearly describes the separate joint, separate technique, and separate clinical indication. Claims are often denied when the record lacks anatomical specificity or when modifier 59 is used to bypass bundling rules without adequate justification.
RT and LT — Laterality Modifiers
Laterality modifiers are essential when billing unilateral joint injections. RT indicates the right side and LT indicates the left side. When a provider performs injections in two different joints on opposite sides of the body—such as the right knee and left shoulder—each line item must reflect the correct RT/LT designation. Many Medicare contractors prefer RT/LT for bilateral claims instead of modifier 50, so payer policy review is required.
Modifier 80 — Assistant Surgeon
Modifier 80 is used when an assistant surgeon is medically necessary for the procedure. Although uncommon for standard arthrocentesis, it may apply in circumstances where the aspiration or injection is part of a more involved surgical procedure or when assistance is required to safely position or stabilize the joint. Modifier 80 typically results in an additional assistant-surgeon payment calculated as a percentage of the primary surgeon’s allowable amount. Coverage varies by payer, and documentation must explain why assistance was medically necessary.
Modifier 22 — Increased Procedural Services
Modifier 22 may be reported when the procedural work exceeds the typical effort required for 20610, such as when significant joint edema, severe synovitis, or complex fluid aspiration requires prolonged or technically difficult manipulation. This modifier triggers manual review, and supporting documentation must clearly detail the increased work compared to a typical arthrocentesis.
Modifier 76 and 78 — Repeat or Related Services
Modifier 76 is used when the same provider repeats the same procedure on the same day. Modifier 78 may apply when a patient returns for related procedural care within the global period (though 20610 has a zero-day global). These modifiers often apply in infectious, inflammatory, or post-surgical joint management scenarios where repeated aspirations are clinically indicated.
Reasons for Denials WITH 20610 CPT
Payers frequently deny 20610 when documentation fails to clearly identify the joint treated, the reason for aspiration or injection, or the medication administered. Other denials arise from incorrect or missing modifiers when multiple joints are treated on the same day, lack of justification for imaging guidance, or billing 20610 alongside evaluation and management codes without supporting distinct documentation. Claims may also deny when the diagnosis does not support medical necessity—for example, attempting to bill a major joint aspiration with a non-specific or unrelated ICD-10 code. Tools like Virtual Examiner® and Virtual AuthTech help organizations identify bundling conflicts, missing documentation elements, and high-risk adjudication issues before the claim is submitted.
PCG Software’s Authority and Expertise in CPT Code Interpretation
For more than 30 years, PCG Software has supported payers, MSOs, IPAs, TPAs, and clinical organizations in improving claims accuracy, preventing fraud and waste, and strengthening compliance around high-volume procedure codes such as 20610. Our solutions—including
Virtual Examiner®,
VEWS™, Virtual AuthTech, and
iVECoder®—apply payer-side adjudication logic, NCCI rules, and multi-year episode-of-care analytics to identify coding errors before payment is released. By combining clinical insight with rule-based automation, PCG helps organizations reduce improper payments, enhance operational efficiency, and maintain full compliance across musculoskeletal and orthopedic claims workflows.
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others