CPT 99386 - Adult Preventive Visit Billing
Quick Summary of CPT Code 99386
CPT
99386 represents a
preventive medicine evaluation for a new patient aged 40–64, covering comprehensive risk assessment, age-appropriate screenings, counseling, and anticipatory guidance. Unlike problem-oriented visits such as 99203, this code is used specifically for a preventive exam that does not address a chief complaint. Because preventive care is covered differently across payers and is often reimbursed at 100% under ACA rules, documentation must precisely match preventive visit criteria. Claims examiners carefully review 99386 to ensure the service was not problem-focused, that risk assessments were completed, and that time-based coding was not used incorrectly. This guide explains who bills 99386, when it should be used, the documentation required, and the most common reasons for denials.
The Who, What, When for billing and paying for CPT Code 99386
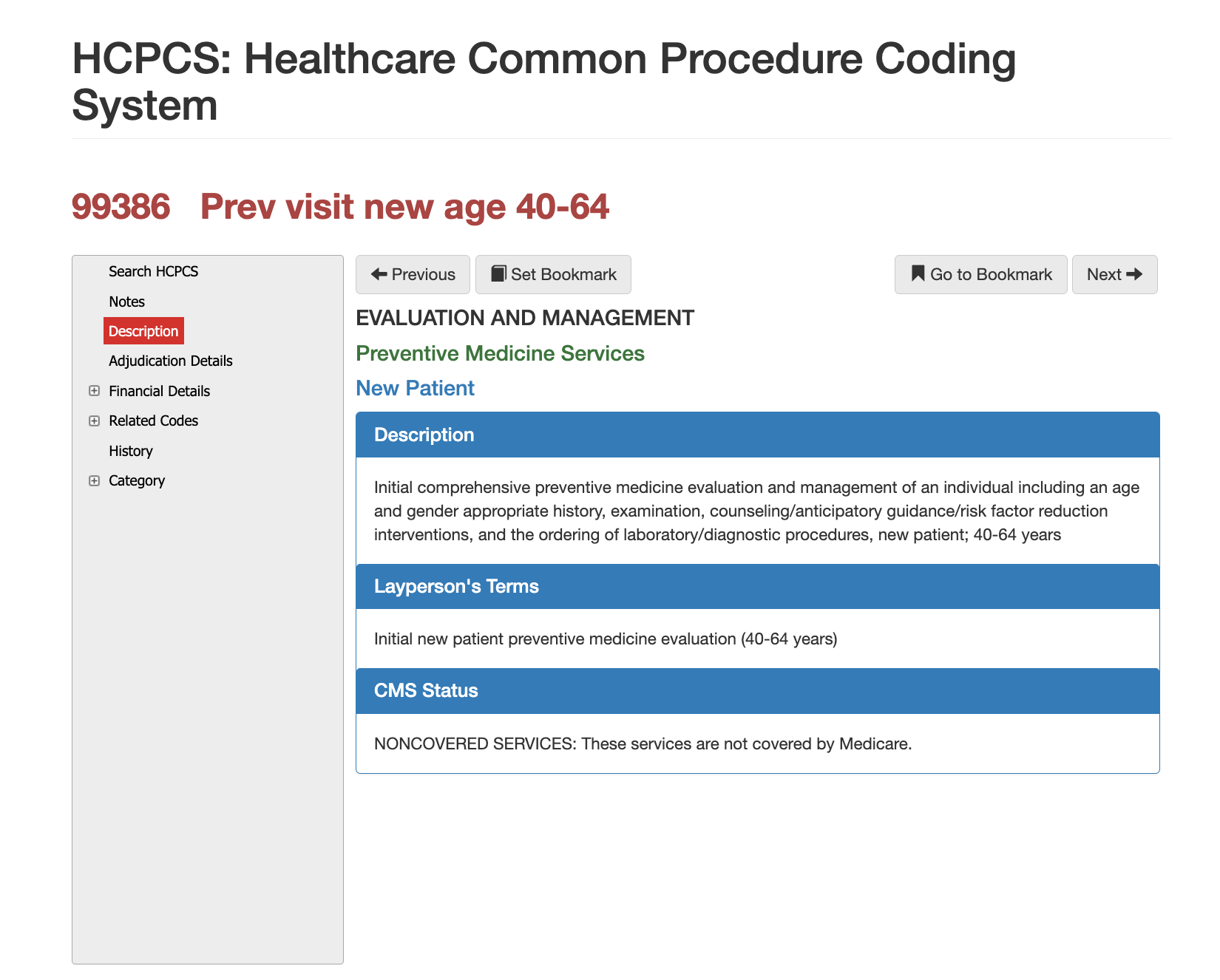
Definition of CPT Code 99386 - AMA vs Layperson:
The AMA defines 99386 as a comprehensive preventive evaluation and management service for a new patient aged 40–64. This includes a complete medical history, physical examination, counseling on disease prevention, and the ordering of appropriate diagnostic services. The service is not tied to medical decision-making or time; instead, it reflects the scope and comprehensiveness of the preventive exam.
In plain language, 99386 is a physical exam for new adult patients in midlife. It focuses on screening, prevention, lifestyle counseling, and identifying undiagnosed risk factors—not diagnosing or treating active medical problems.
When is CPT Code 99386 Used?
CPT 99386 is used when a clinician performs a dedicated preventive visit, meaning the purpose of the encounter is to evaluate the patient’s overall health, identify risk factors, perform recommended screenings, and provide health education. The visit must be entirely preventive in nature. If a patient presents with an acute concern or a worsening chronic condition, the provider must address the issue separately under an E/M code such as 99203, often requiring modifier 25.
Claims reviewers verify that the documentation describes:
- A full preventive exam
- Age-appropriate screenings
- Lifestyle or risk counseling
- Immunization review
- Family and social history relevant to prevention
- Anticipatory guidance
Payers deny 99386 when the note reflects problem-focused care or when the documentation lacks evidence of comprehensive preventive services.
Who bills for CPT Code 99386?
Primary care physicians, internal medicine providers, OB/GYNs, and family physicians account for the majority of 99386 billing. Preventive visits are also commonly performed by nurse practitioners and physician assistants in medical homes, FQHCs, and outpatient primary care settings. Because this code represents a new-patient comprehensive preventive evaluation, payers often review whether the clinician is credentialed for preventive services and whether the patient meets age and new-patient status requirements.
Top Diagnosis ICD-10 for CPT 20220
Preventive visits, such as 99386, require a Z-code as the primary diagnosis. Common examples include:
- Z00.00 – General adult medical exam without abnormal findings
- Z00.01 – Adult medical exam with abnormal findings
- Z13.xx – Screening codes for metabolic, endocrine, cardiovascular, or cancer risk
When abnormal findings are identified, secondary problem-oriented diagnoses may be included. However, these secondary conditions do
not convert the visit into a problem-focused E/M service if the primary intent remains preventive. Claims examiners look for clear differentiation between preventive and diagnostic work, especially when modifier 25 is used.
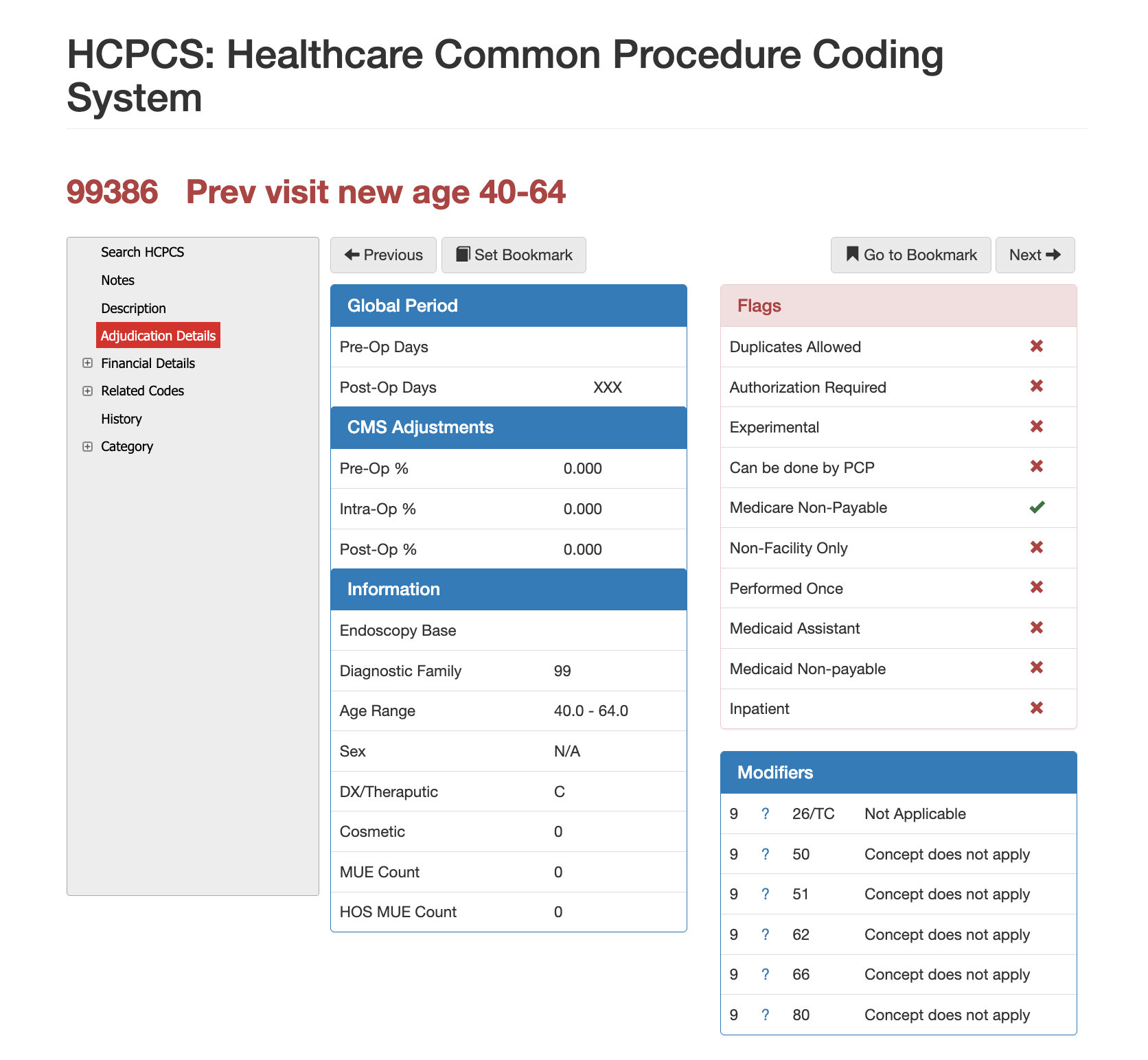
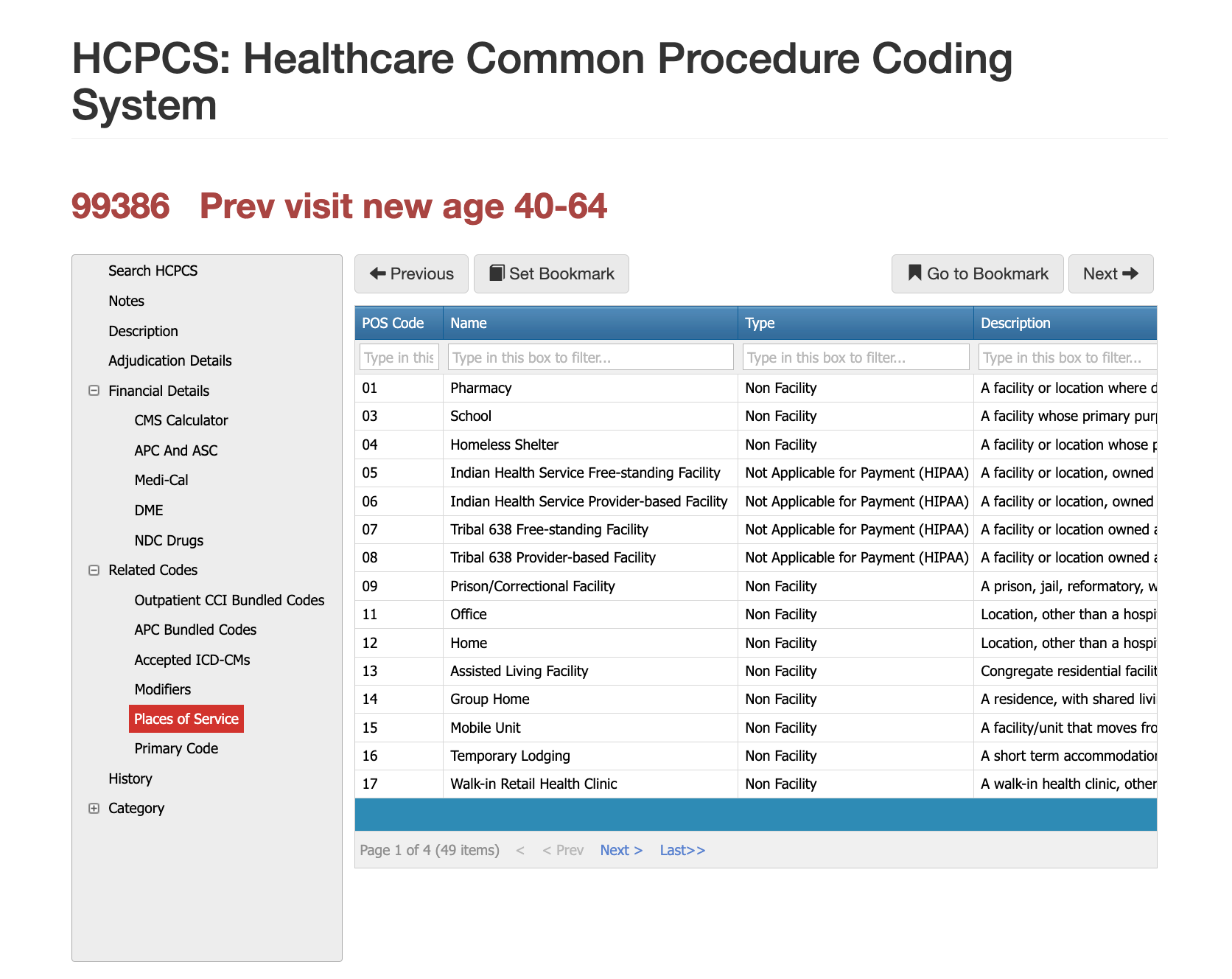
Places of Service for CPT Code 20220
CPT 99386 is typically billed in outpatient settings such as primary care clinics, internal medicine offices, OB/GYN practices, and FQHCs. It is not appropriate in emergency departments, inpatient settings, or observation units because preventive services exclude acute, urgent, or hospitalization-based care. Claims reviewers confirm that the POS supports a preventive visit and that payer rules do not restrict preventive coverage to specific sites.
Proper Documentation for CPT Code 99386
To support 99386, the medical record must show that a full preventive evaluation was performed. This includes a comprehensive systems-based history, age-appropriate physical examination, assessment of risk factors, counseling on health behaviors, screening recommendations, and preventive planning. Providers should document discussions about tobacco use, diet, exercise, alcohol use, mental health screening results, cancer screening schedules, and immunization status. The visit must clearly reflect that the purpose was preventive, not problem-oriented. If both preventive and problem-focused care occur, the documentation must distinguish them clearly to justify additional E/M billing. Lack of breadth in documentation is the most common reason payers deny 99386 or recode it to a problem-based visit.
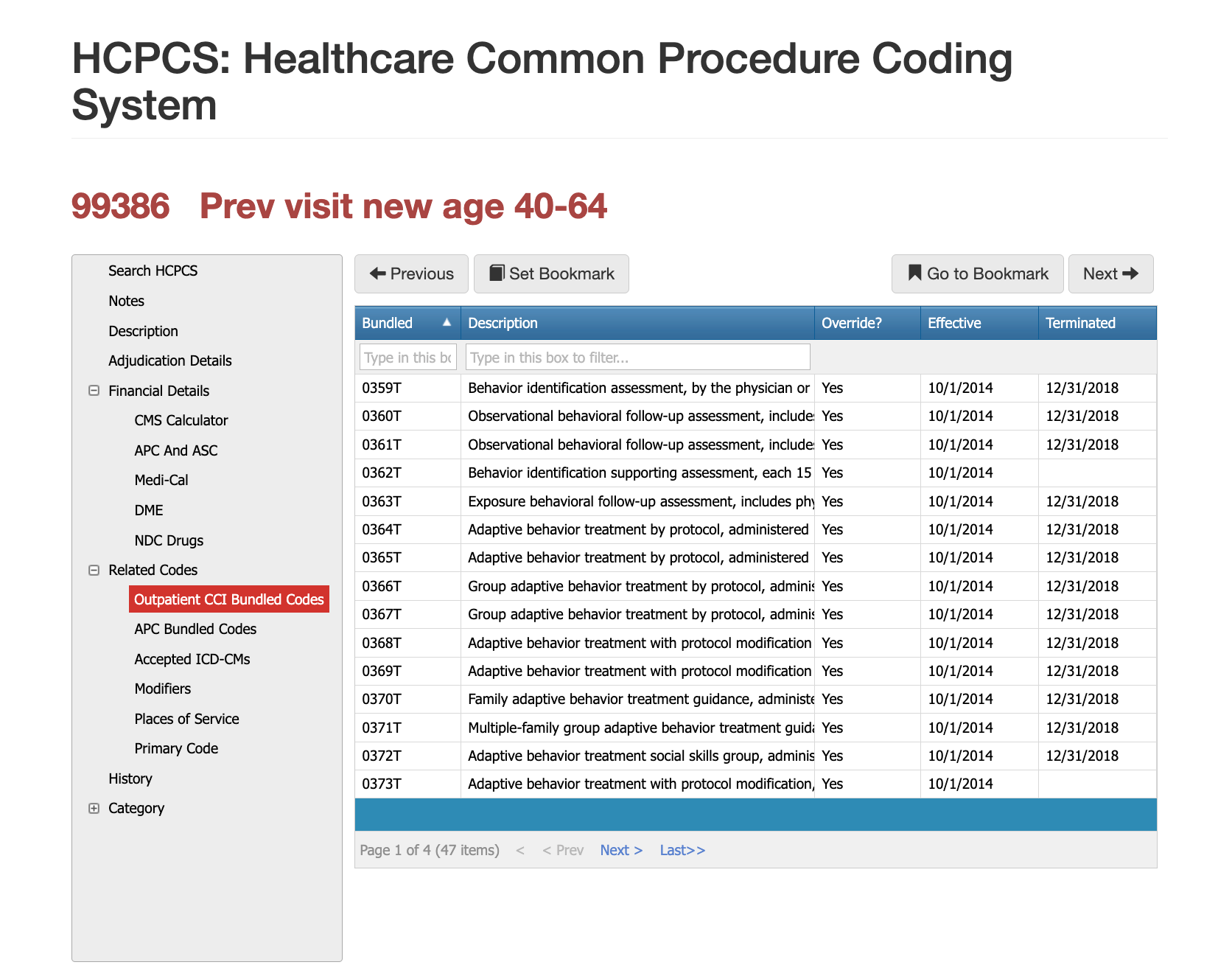
Related CPT Codes for 20220
CPT 20220 sits within a family of musculoskeletal biopsy codes that differ primarily by the depth of access, technique, and anatomical complexity. CPT 20225, which represents a deep bone biopsy, is used when the provider must dissect through deeper tissues or when the bone site is not readily accessible by superficial approach. Open surgical biopsy codes in the 20100 series apply when bone must be surgically exposed rather than accessed percutaneously. Imaging guidance codes may also be used when radiologic assistance is documented. Understanding these distinctions is essential because incorrect code selection can lead to significant overpayment or underpayment.
| Code | Description | How It Compares to 99386 |
|---|---|---|
| 99396 | Preventive visit, established patient (40–64 years) | Used for established patients; 99386 is strictly for new patients. |
| 99386–99387 | Preventive visits for older adults | Age-dependent codes; 99386 covers midlife adults only. |
| 99203 / 99204 | New patient problem-focused E/M visits | Used when the primary purpose is diagnosis or management rather than prevention. |
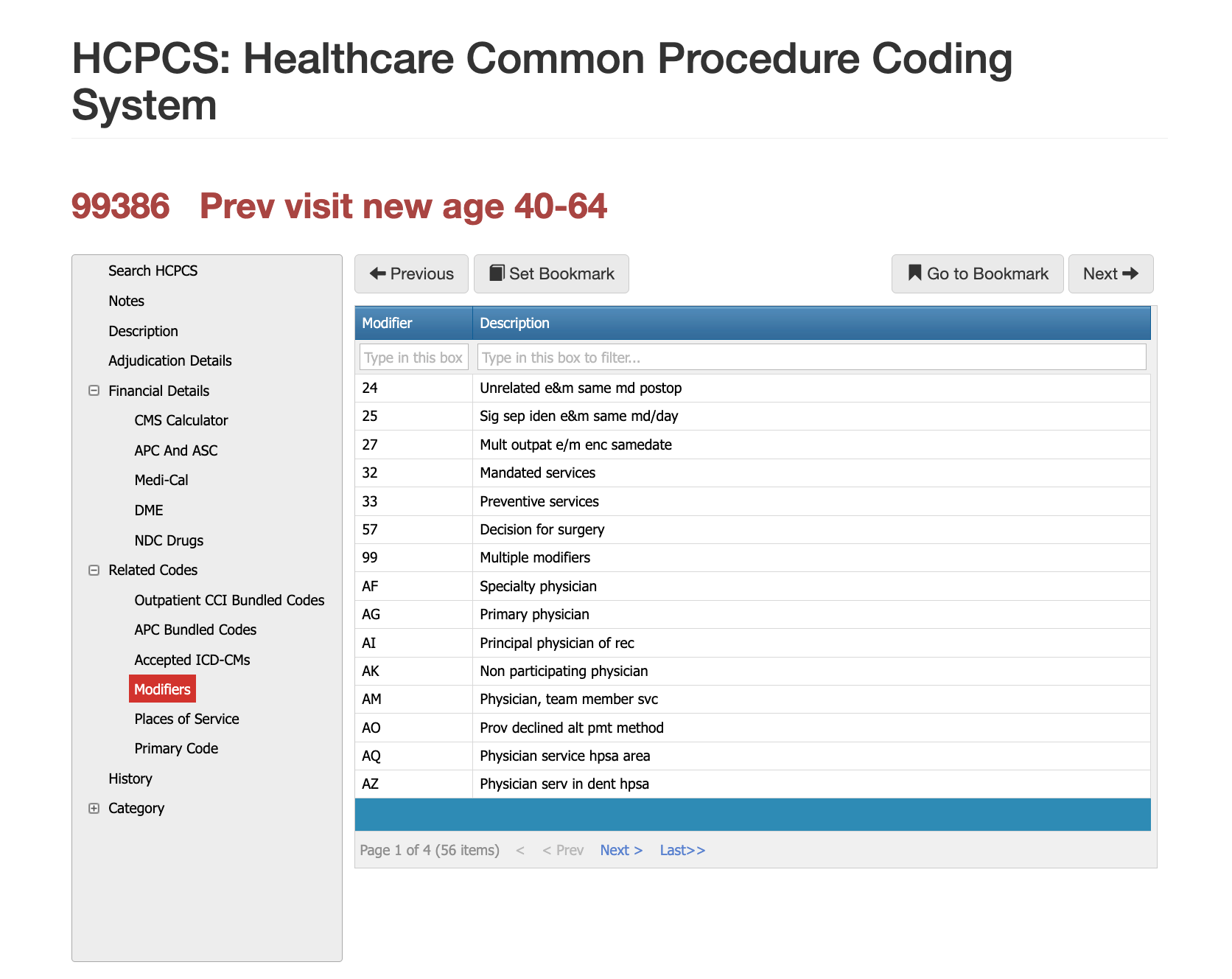
Modifier 25 – Preventive Visit + Problem-Focused E/M
Modifier 25 is used when a provider performs a preventive exam and a medically necessary problem-oriented E/M service at the same visit. Documentation must clearly separate preventive elements from problem-focused assessment and demonstrate that the issue required significant additional work.
Modifier 33 – Preventive Service
Some payers require Modifier 33 to signal that the service is preventive and eligible for cost-sharing elimination under ACA standards. It should only be appended when payer rules explicitly require it.
Modifier 95 – Telehealth (Limited Use)
While rare for preventive exams, some commercial plans allow partial preventive services via telehealth with modifier 95. Most payers still require in-person exams for full preventive billing.
Most Common Reasons for 20220 CPT Denials
Payers frequently deny 99386 when documentation is not comprehensive enough to justify a preventive visit or when the encounter focuses primarily on acute problems. Denials also occur when the primary diagnosis is not a Z-code, when the patient does not qualify as a new patient under CPT’s three-year rule, or when the POS is not consistent with preventive services. Claims may be recoded to 99203 or denied entirely when the documentation resembles problem-oriented care without clearly documented preventive components.
RVU Negotiation Guide for CPT 20220
Reimbursement for 99386 is based on its assigned RVUs, which reflect the extensive work, time, and practice expenses associated with a comprehensive preventive exam. Preventive visits often reimburse at higher rates than problem-oriented visits because they involve broader evaluation and long-term health planning. Using Virtual AuthTech or iVECoder allows payers and providers to compare reimbursement at different Medicare percentages, evaluate state-by-state differences via GPCI, and identify when contracted rates fail to reflect true service value. These tools also detect patterns where preventive services are mistakenly coded or downcoded, improving financial accuracy for both sides.
The Easier Way to Research Codes
CPT 99386 is a cornerstone code for adult preventive care and a focus area for payer audits due to its high reimbursement value. Ensuring accurate documentation, selecting appropriate Z-codes, and distinguishing preventive from problem-focused work helps reduce denials and supports long-term compliance. PCG Software’s Virtual Examiner®, VEWS™, Virtual AuthTech, and iVECoder® platforms assist both payers and providers in validating preventive visit criteria, identifying documentation gaps, and maintaining consistent coding accuracy across outpatient settings. Preventive care only delivers value when billed correctly, and PCG’s tools ensure it stays compliant, efficient, and defensible.
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others