J799 CPT - Compound Drug, Unclassified Codes for Drugs
J7999 Quick Summary
HCPCS Code J7999 is a miscellaneous code used to report drugs, biologicals, or radiopharmaceuticals that do not have a specific HCPCS code assigned. It is typically used for unlisted drugs, biologicals, or radiopharmaceuticals that are not covered by any other existing HCPCS code. J7999 allows providers to report these products for reimbursement purposes when no other more specific code is available. However, because of its generic nature, J7999 can be challenging to use correctly and can result in billing errors or denials if not properly documented and coded.
The Who, What, When for billing and paying for CPT Code J7999
ADefinition of CPT Code J7999 - AMA vs Layperson:
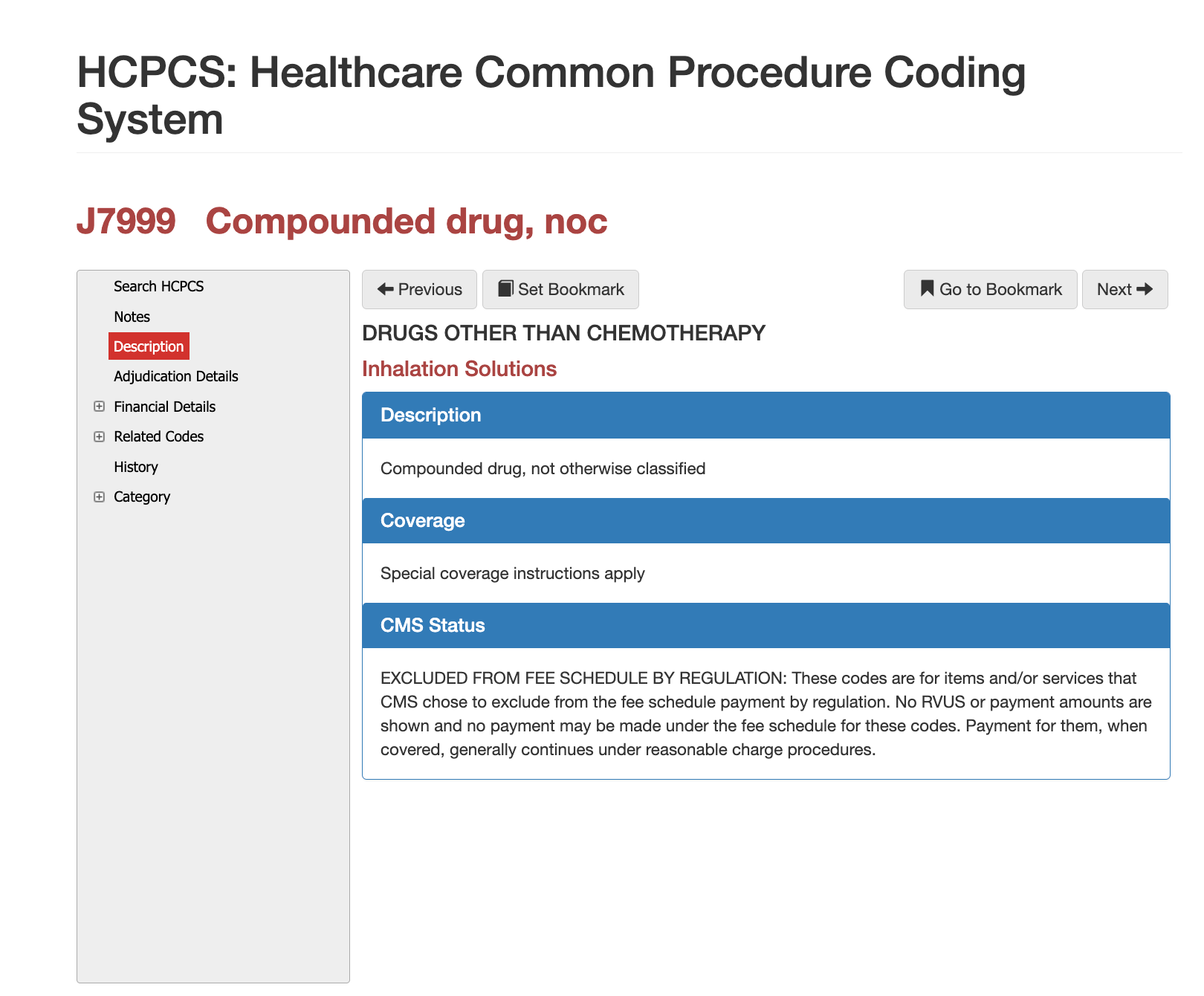
CMS defines
J7999 as “unclassified drugs, other than chemotherapy drugs classified under J9999.” This means the code is used strictly when no other HCPCS J-code accurately describes the drug being administered. In plain language, J7999 functions as a placeholder code for medications that do not yet have an official billing code. This often occurs with newer pharmaceuticals awaiting CMS classification, compounded drugs prepared in the facility, or low-volume medications that never receive a permanent code.
When is CPT Code J7999 Used?
J7999 is appropriate only when the administered medication lacks a specific HCPCS code. Claims reviewers expect the clinical note or pharmacy label to clearly indicate that a permanent J-code does not exist. The code is commonly used for compounded drug mixtures, new medications recently released to the market, or medications administered off-label where established J-codes do not apply. Providers must ensure that documentation justifies not only the drug administration but also the absence of an alternative HCPCS code, since payers frequently deny J7999 when a more specific code should have been reported.
Who bills for CPT Code J7999?
There is no fixed diagnosis list for J7999 because it is not tied to a specific therapeutic class. Instead, the diagnosis must align with the medical purpose of the drug administered. Claims reviewers assess whether the diagnosis clearly supports drug administration, and whether the medication documented is clinically appropriate for the condition. Diagnoses commonly associated with J7999 include acute and chronic pain conditions, post-operative inflammation, dermatologic lesions requiring office-based injections, ENT and ophthalmologic conditions requiring medicated solutions, and musculoskeletal disorders treated with pharmacologic agents. Inconsistent or vague diagnoses often trigger payer requests for additional records or result in outright denial.
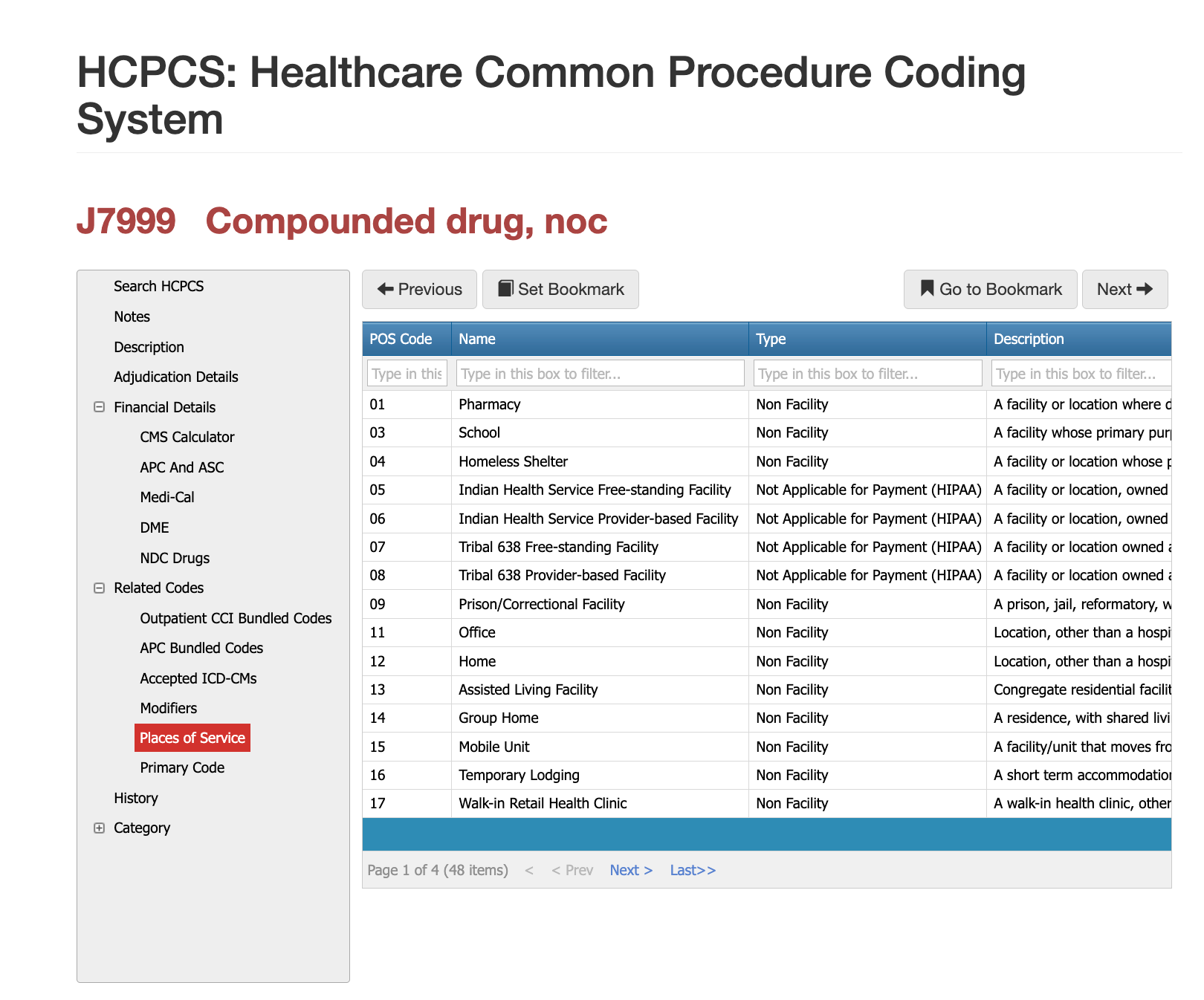
Places of Service for CPT Code 20220
J7999 is used across numerous outpatient settings. Physician offices represent the most frequent place of service, particularly when administering medications during minor procedures or injections. Hospital outpatient departments and ambulatory surgery centers also report J7999 whenever on-site pharmacies prepare or dispense a drug without an established HCPCS code. Urgent care centers, independent clinics, and federally qualified health centers may bill J7999 when non-standard medications are used in treatment. Claims examiners review POS codes closely to ensure the drug administration setting matches payer expectations and billing rules. Documentation must clearly support that the medication was administered in the reported location and that the corresponding procedural code, if any, was also appropriate for that site.
Proper Documentation for CPT Code 20220
Because J7999 lacks specificity, documentation is the determining factor in whether a claim is paid or denied. The medical record must include the exact drug name, strength, dosage, concentration, lot number (if applicable), route of administration, and the clinical rationale for use. Payers also expect the National Drug Code (NDC), the number of units billed, and a clear calculation showing how the billed quantity relates to the documented dose. In many cases, payers require a copy of the pharmacy invoice to confirm acquisition cost, particularly when the drug is compounded. Documentation should also support medical necessity, demonstrating that the drug administered is clinically appropriate for the diagnosis and that no alternative code applies. Missing or incomplete information is the most common cause of denials under J7999.
Related CPT Codes for 20220
The following table outlines how J7999 compares with related miscellaneous drug codes and clarifies when each code should be used. This helps reduce miscoding and avoid denials caused by incorrect unclassified drug reporting.
| Code | Description | How It Differs From J7999 |
|---|---|---|
| J3490 | Unclassified drugs | Similar function, but J3490 is used more commonly for standard office-administered drugs; some payers prefer J3490 over J7999. |
| J9999 | Not otherwise classified chemotherapy drugs | Used strictly for antineoplastic drugs; should not be confused with non-chemotherapy miscellaneous drugs billed under J7999. |
| C9399 | Unclassified drugs or biologics (hospital outpatient use) | Hospital outpatient equivalent; not used in physician offices or ASC settings. |
| J7999 | Unclassified, non-chemotherapy drugs | The correct code when no specific HCPCS J-code exists for a non-chemotherapy drug. |
Avastin J7999 as an example
Avastin is created by the Pharmaceutical Manufacturer, Genentech. Avastin is an anti-angiogenic therapy (tumor-saving) use alongside chemotherapy to prevent tumor growth. To find out more about the drug you can utilize iVECoder or Virtual AuthTech through PCG Software, or you can visit Genentech.
Avastin Non-Ophthamologic Use and HCPCS
- Avastin for J9035 for non-opthamologic use (10mg).
- Q5017 for biosimilar (MVASI; 10mg).
- HCPCS Q5118 for biosimilar (ZIRABEV; 10mg).
- Effective 1/1/23; HCPC Q5126 for biosimilar (ZIRABEV; 10mg).
- Effective 1/1/23; HCPCS Q5129 for Vegzelma.
Avastin Ophthamologic Use and HCPCS
- Part B MAC should be C9142, J9035, Q5017, or Q5118 (billed for one eye).
- ASC (ambulatory) should be C9257 (0.25mg; injection) when within the surgical center setting.
- ALYMSIS (biosimilar; 10mg) should be used with Q5126 per 1/1/2023.
- MVASI (biosimilar; 10mg) should be used with Q5107 per 1/1/2023.
- ZIRABEV (biosimilar; 10mg) should be with Q5118 per 1/1/2023.
Avastin RT, Avastin LT, Avastin 50
If intravitreal injection uses CPT 67028 with site modifier (RT, LT, or 50) to indicate if performed unilaterally or bilaterally. Without this modifier, you will likely be denied.
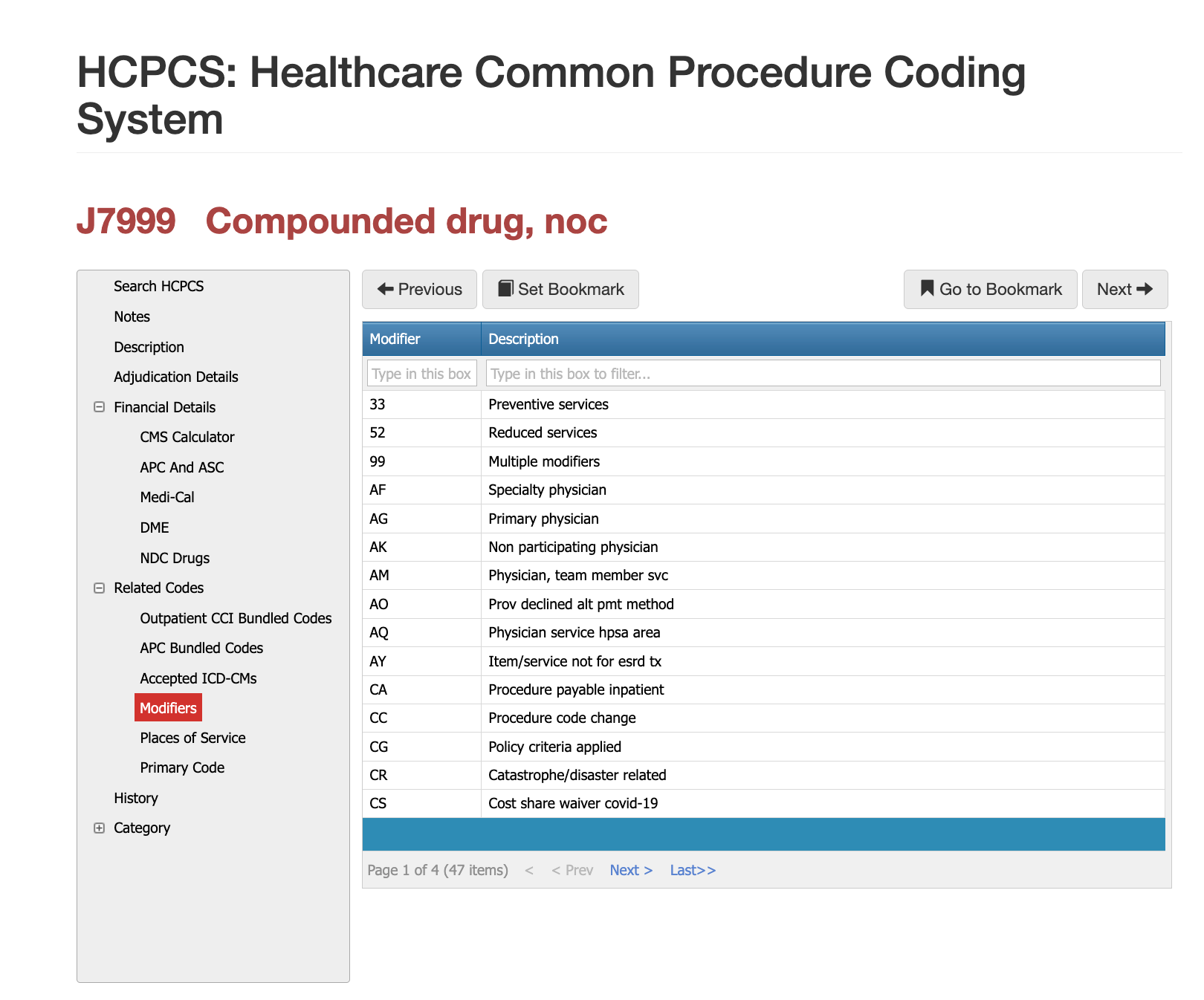
Modifier Guidance for CPT Code 20220
J7999 rarely requires modifiers, but certain situations make them appropriate. Modifier
JW may be used when documenting discarded drug amounts, provided the payer accepts JW reporting for unclassified drug codes. Modifier
JZ may apply for Medicare when no discarded drug remains. Some payers also allow the
CG modifier when the drug is part of a comprehensive outpatient payment under OPPS packaging rules. Because modifier acceptance varies significantly, payers often request clarification whenever modifiers appear on J7999 claims. Providers should consult individual payer policies before appending any modifier to this code.
Most Common Reasons for 20220 CPT Denials
J7999 denials typically occur when required drug details are missing or unclear. Payers commonly deny claims that lack the drug name, NDC, dosage, or invoice documentation. Denials also arise when the diagnosis does not justify drug administration, when a more specific HCPCS code exists and should have been used, or when units billed do not match the documented dose. Pricing disputes are particularly common because unclassified drug reimbursement often requires manual review and cross-checking against acquisition cost. Clear, complete, and consistent documentation prevents most denials.
The Easier Way to Research codes
For more than 30 years, PCG Software has supported Health Plans, MSOs, IPAs, TPAs, and provider organizations in improving coding accuracy, strengthening compliance, and reducing fraud, waste, and abuse. Our solutions, including Virtual Examiner®, VEWS™, and iVECoder®, are built on decades of payer-side adjudication experience and reflect the same logic used by health plans nationwide. National regulatory guidance, payer policies, compliance standards, and large-scale claims review patterns inform this CPT 69210 analysis.
Toss out the CPT book.
Stop researching articles.
Sign up for iVECoder today!
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others