Incorrect Gender and Diagnosis Codes - Impact on Providers and Payers
Summary: Incorrect diagnosis and gender coding is fundamentally a data integrity problem, not just a billing or quality reporting issue. These errors first impact encounter data, which then flows downstream into HEDIS scores, risk adjustment, quality reporting, audits, and reimbursement decisions.
Understanding the differences between encounter data and HEDIS—and how errors can propagate between them—is essential for healthcare providers and payers seeking to reduce denials, improve compliance, and protect their financial and reputational standing.
This article explains how incorrect diagnosis and gender coding corrupts encounter data, how that corruption distorts HEDIS performance, and why preventing errors at the encounter level is far more effective than reacting to denials or poor quality scores after the fact.
Encounter Data vs Hedis
Although encounter data and HEDIS are often discussed together, they serve fundamentally different roles within the healthcare data lifecycle. Encounter data represents the raw clinical and administrative record of care delivered. It includes diagnoses, procedures, patient demographics, dates of service, places of service, and provider identifiers. This data is used for claims adjudication, risk adjustment, quality reporting, actuarial analysis, and regulatory oversight.
HEDIS, by contrast, is not a data source but a measurement framework built on encounter and claims data. HEDIS evaluates whether specific populations received defined evidence-based care, using existing data already submitted by providers and processed by payers. When encounter data is inaccurate, HEDIS results will also be inaccurate, even if the underlying clinical care was appropriate. Encounter data is the foundation; HEDIS is an analytical outcome derived from it.
Why Encounter Data Accuracy Comes First
Errors in diagnosis and gender coding compromise encounter data at the point of creation. Once submitted, this flawed data propagates across payer systems, analytics platforms, and reporting programs, often without triggering immediate payment denials or alerts. Many encounter-level errors are silently accepted and stored, only surfacing later during audits, quality reviews, or regulatory examinations.
This is what makes encounter data errors particularly dangerous. Unlike claim denials, which provide direct and timely feedback, encounter data inaccuracies can persist unnoticed for months or years. By the time issues appear, they are often embedded across multiple datasets, making correction costly, time-consuming, and operationally disruptive.
Preventing Errors at the Encounter Level
Preventing downstream compliance and quality issues requires addressing errors where they originate: at the encounter and documentation stage. Ensuring consistency across EHRs, practice management systems, and payer submissions is critical. Diagnosis, procedure, and demographic data must align logically and clinically before claims are submitted and encounter data is finalized.
Relying solely on payer denials or clearinghouse edits is insufficient. Many encountered data issues are paid and never flagged. Proactive internal monitoring and validation of encounter data is far more effective than reactive correction after the fact.
Examples of Incorrect Sex and Diagnosis
PSA on Female
A prostate-specific antigen (PSA) test billed for a female patient is a common example of a gender-diagnosis mismatch that should be flagged at the encounter level. PSA testing is clinically associated with prostate tissue, and in the absence of documented gender reassignment, intersex conditions, or specific clinical modifiers, this encounter represents invalid demographic alignment. While such claims may occasionally pass initial adjudication, they create encounter data contamination that can surface later in audits, quality reporting anomalies, or compliance reviews. These errors illustrate why demographic validation must occur before encounter data is finalized.
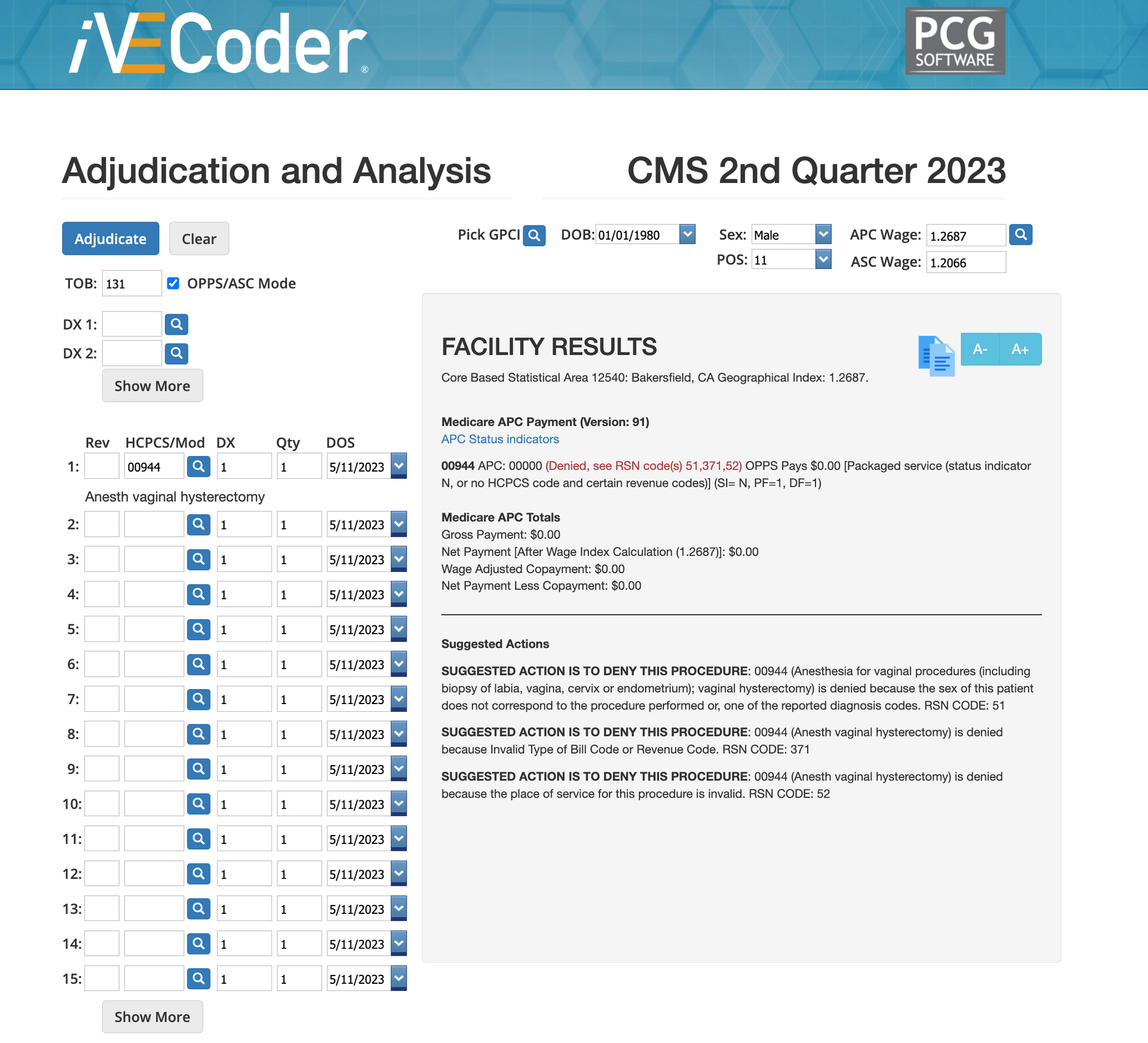
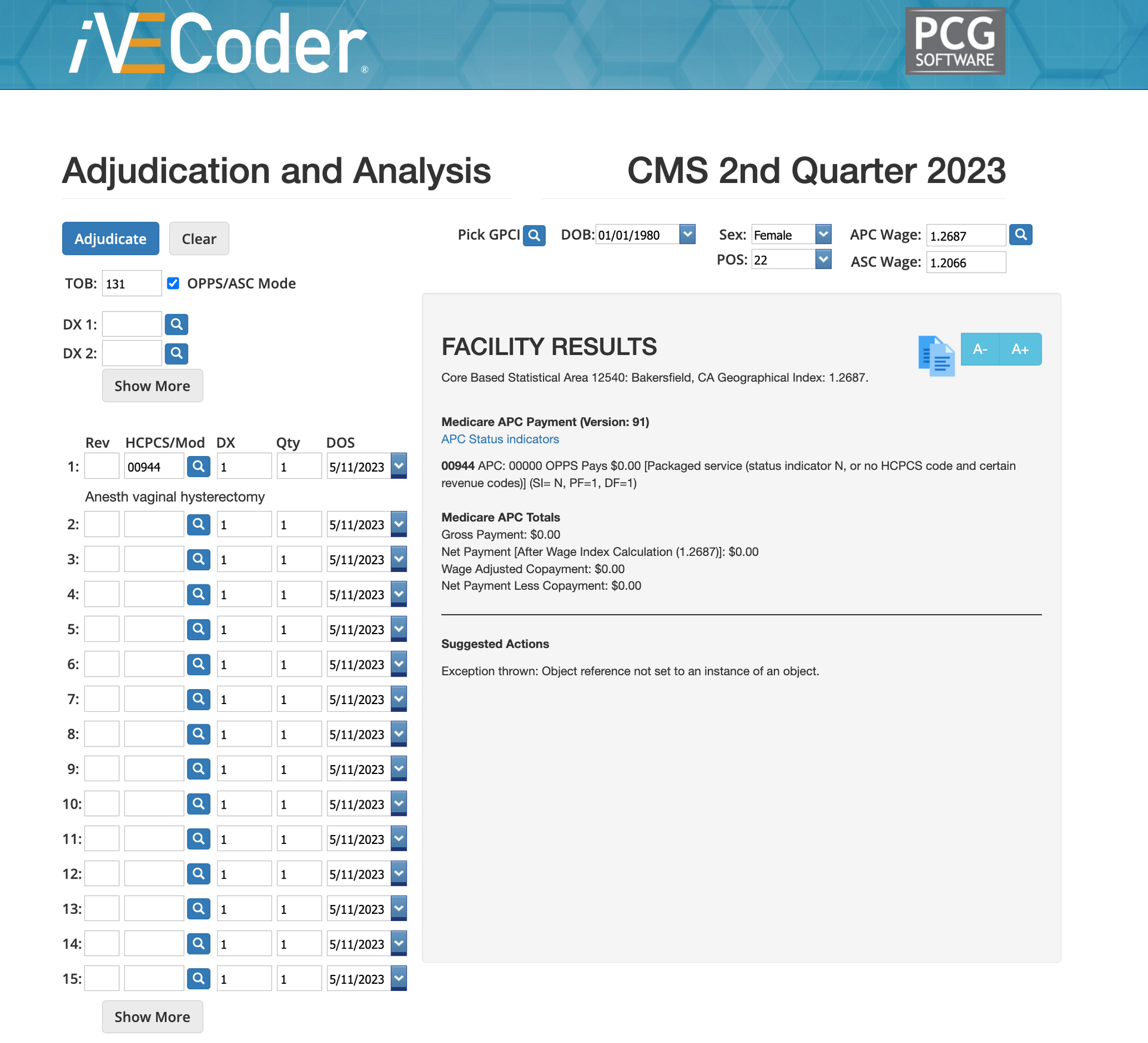
Hysterectomy Billed for Male Patient
A hysterectomy billed under a male patient record represents a clear gender-procedure conflict and is typically indicative of demographic data entry errors or incorrect patient selection at the encounter stage. These errors frequently occur during registration or when patient records are duplicated or merged incorrectly. If not corrected prior to submission, such encounters may be denied or, worse, paid and later identified during retrospective audits, creating unnecessary compliance exposure.
Cervical Cancer Screening Billed for Male Patient
Cervical cancer screening procedures billed for a male patient are another example of encounter-level demographic mismatch that should be identified before claim submission. These errors often result from incorrect patient selection, template misuse, or incomplete demographic updates within the EHR. While typically denied quickly, repeated occurrences can signal systemic workflow issues and may increase payer scrutiny or trigger targeted audits.
We've seen this the most when there is a husband and wife both being treated by the same clinic or physician.
Examples You'll have to look at the documentation to determine
Circumcision for Mother
Circumcision billed for a newborn male should not be misinterpreted as an error when the mother is listed as the guarantor or subscriber on the claim. In this scenario, the procedure is correctly associated with the infant patient, not the adult subscriber, and reflects a valid family billing structure. Mistaking this relationship for a gender-procedure conflict can lead to inappropriate denials or incorrect internal flagging. This example highlights the importance of distinguishing patient-level demographics from subscriber or guarantor data when evaluating encounter accuracy.
Testosterone Therapy Billed for Female Patient
Testosterone therapy billed for a female patient is not automatically a gender-coding error and requires careful documentation review to determine validity. While testosterone is commonly associated with male hypogonadism, it may be clinically appropriate for certain female patients, including those with documented endocrine disorders, post-oophorectomy hormone management, or gender-affirming care. Without reviewing the clinical notes, diagnosis context, and treatment intent, this encounter could be incorrectly flagged or denied. This example underscores why demographic alignment checks must be paired with documentation validation rather than applied as absolute rules.
Mastectomy Billed for Male Patient
A mastectomy billed for a male patient may initially appear to be a gender-procedure mismatch, but documentation review is essential before determining error. Male patients may undergo mastectomy for conditions such as breast cancer, gynecomastia with medical necessity, or other clinically supported indications. In these cases, the procedure is appropriate despite deviating from common gender associations. Automatically classifying such encounters as errors without reviewing diagnosis codes, pathology reports, and operative notes can result in improper denials and inaccurate encounter data classification.
How to Avoid Wrong Sex Denials and Encounter Data Clean-ups
AI Detection of Incorrect Coding
As coding rules, payer policies, and regulatory expectations continue to evolve, manual review processes cannot scale effectively. Artificial intelligence has become an essential tool for identifying encounter-level risks before they cascade into claims, HEDIS reporting, and audits.
AI-driven systems can evaluate diagnosis, procedure, and demographic alignment in real time, flagging inconsistencies that may violate CMS, AMA, or payer-specific logic. These tools help organizations strengthen data integrity, support staff education, and reduce the likelihood of denials, audit findings, and quality score degradation.
Before AI Medical Coding Scrubbers
After AI Medical Coding Scrubbers
Summary of Wrong Sex Denials
Encounter data is the backbone of modern healthcare payment, analytics, and quality measurement. Errors at this level silently undermine HEDIS scores, financial performance, and regulatory confidence. Organizations that focus solely on HEDIS outcomes without addressing encounter data integrity are treating symptoms rather than root causes. Accurate encounter data is foundational to compliant billing, reliable quality measurement, and sustainable healthcare operations. Addressing these issues proactively protects both providers and payers from unnecessary risk while ensuring that reported performance accurately reflects the care delivered.
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
Free Payer Claims Audit
Complete the form, and we'll contact you to schedule an introductory meeting and discuss our FREE 3-year claims audit to identify areas for cost containment and compliance.
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others