Comparing Modifier 51, 59 and X
Definitions, Case Usage, and Compliance
Modifier 51, modifier 59, and the X modifiers are among the most misunderstood tools in medical billing. Although they are often used interchangeably, each modifier serves a distinct purpose in payer adjudication logic. This guide explains when each modifier should be used, how payers interpret them, common compliance risks, and real-world claim scenarios that trigger denials or payment reductions.
How are Modifiers 51, 59, and X, similar and different?
Modifiers
51, 59, and the X modifiers (XE, XP, XS, XU) all exist to explain why more than one service appears on the same claim, but they solve different problems in claims adjudication. Modifier
51 addresses payment sequencing when multiple procedures are performed in the same session and tells the payer which service is primary versus secondary for reimbursement reduction—it does
not establish clinical distinctness. Modifier
59, by contrast, is a distinct procedural modifier used to override NCCI edits when two services are normally bundled but were legitimately separate, requiring strong documentation support. The
X modifiers refine Modifier 59 by explaining how the services were distinct—whether by encounter (XE), practitioner (XP), organ or structure (XS), or an unusual non-overlapping service (XU). In practice, payers view Modifier 51 as a payment modifier, Modifier 59 as a bundling exception, and the X modifiers as the most precise and compliant way to communicate distinctness—making them increasingly favored in audits, AI adjudication, and modern claims review systems.
Modifier 51 Explained
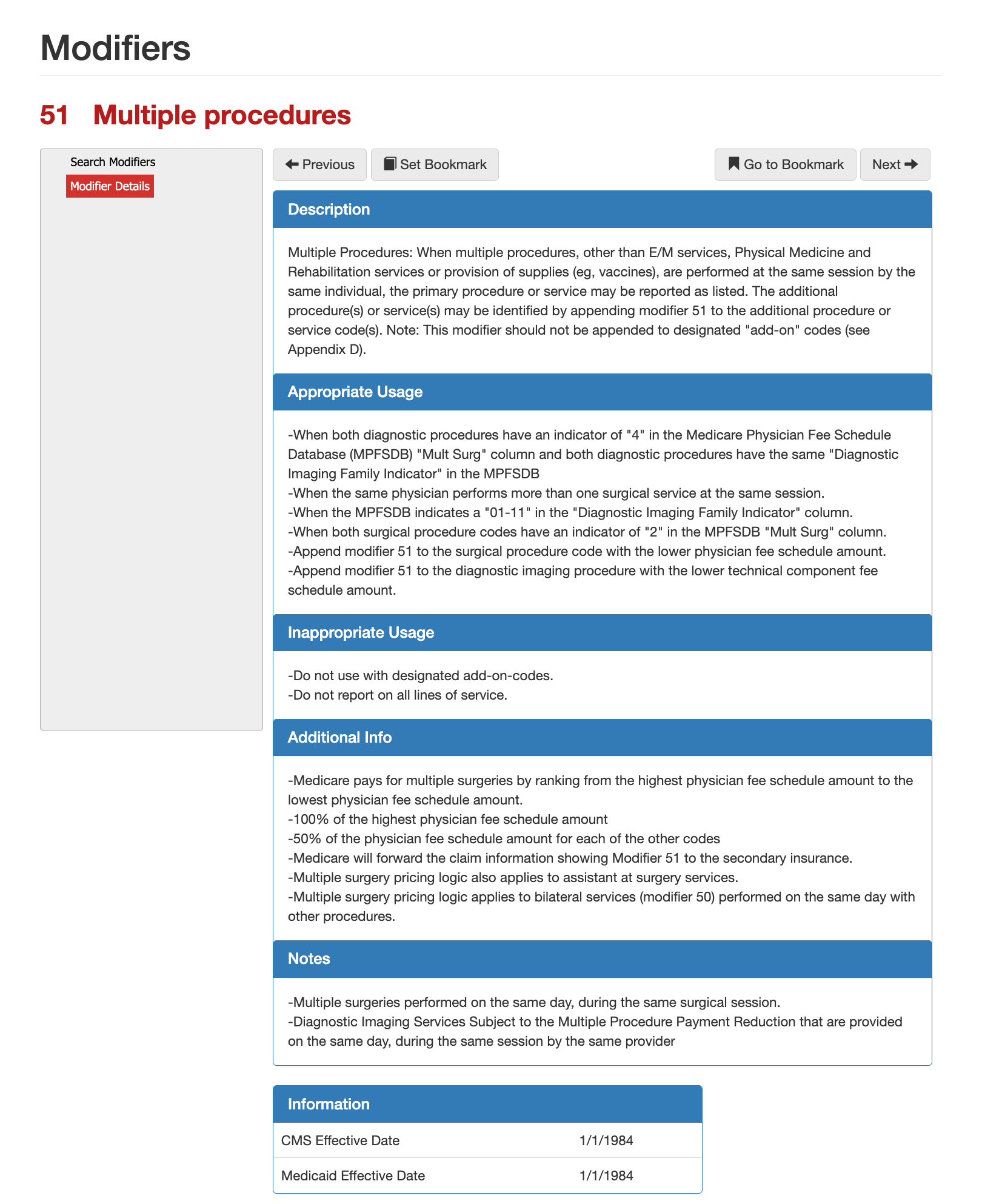
Modifier 51 - Multiple Procedures
Modifier 51 is used to indicate that
multiple procedures—other than E/M services, physical medicine and rehabilitation services, or supplies—were performed during the
same operative session by the
same provider. From a payer perspective, modifier 51 does not justify separate payment for distinct clinical work; instead, it signals that
multiple-procedure payment logic should be applied to secondary services. CMS uses modifier 51 primarily as a
pricing modifier, not a clinical modifier. When reported correctly, it tells the payer to rank procedures by their Physician Fee Schedule amount and apply the standard multiple-surgery reduction methodology rather than paying each procedure at 100 percent.
When is Modifier 51 is Appropriate?
Modifier 51 is appropriate when the same physician performs
more than one surgical procedure during the same session and the additional procedures are
not designated add-on codes. It is commonly applied when both procedures are eligible for multiple-procedure pricing under the Medicare Physician Fee Schedule Database (MPFSDB), specifically when the “Mult Surg” indicator allows reduction. For diagnostic imaging services, modifier 51 may apply when both procedures share the same diagnostic imaging family indicator and are performed during the same encounter. In these cases, CMS applies the multiple procedure payment reduction logic to the technical or professional component, depending on the service type.
When is Modifier 51 not Appropriate?
Modifier 51 should
not be appended to add-on codes, as those services are already priced to be paid separately. It should also not be reported on
every line item of a claim. Only secondary or additional procedures should carry modifier 51, never the primary procedure. Using modifier 51 to override bundling edits or to justify payment for services that are inherently included in a primary procedure is inappropriate and frequently results in claim reductions or post-payment recovery.
When Modifier 51 Affects Payment
Under CMS multiple surgery rules, Medicare pays
100 percent of the highest-valued procedure and
50 percent of the allowable amount for each additional procedure subject to multiple-procedure reduction. This ranking is determined automatically based on the physician fee schedule amounts, not the order in which procedures appear on the claim. Modifier 51 information is also forwarded to secondary insurers, which may apply their own multiple-procedure logic. The same pricing methodology applies to assistant-at-surgery services and may also interact with bilateral services when performed on the same date.
When Modifier 51 Affects Payment
Under CMS multiple surgery rules, Medicare pays
100 percent of the highest-valued procedure and
50 percent of the allowable amount for each additional procedure subject to multiple-procedure reduction. This ranking is determined automatically based on the physician fee schedule amounts, not the order in which procedures appear on the claim. Modifier 51 information is also forwarded to secondary insurers, which may apply their own multiple-procedure logic. The same pricing methodology applies to assistant-at-surgery services and may also interact with bilateral services when performed on the same date.
Modifier 51 Compliance Considerations
From a compliance standpoint, modifier 51 should be used
sparingly and intentionally. Many Medicare Administrative Contractors apply multiple-procedure reductions automatically, meaning modifier 51 may be informational rather than required. Overuse or incorrect placement of modifier 51 is a common indicator of coding pattern risk during audits. Claims examiners expect the medical record to clearly support that multiple distinct procedures were performed during the same operative session and that none of the services are designated as add-on codes or bundled components.
Modifier 59 Explained
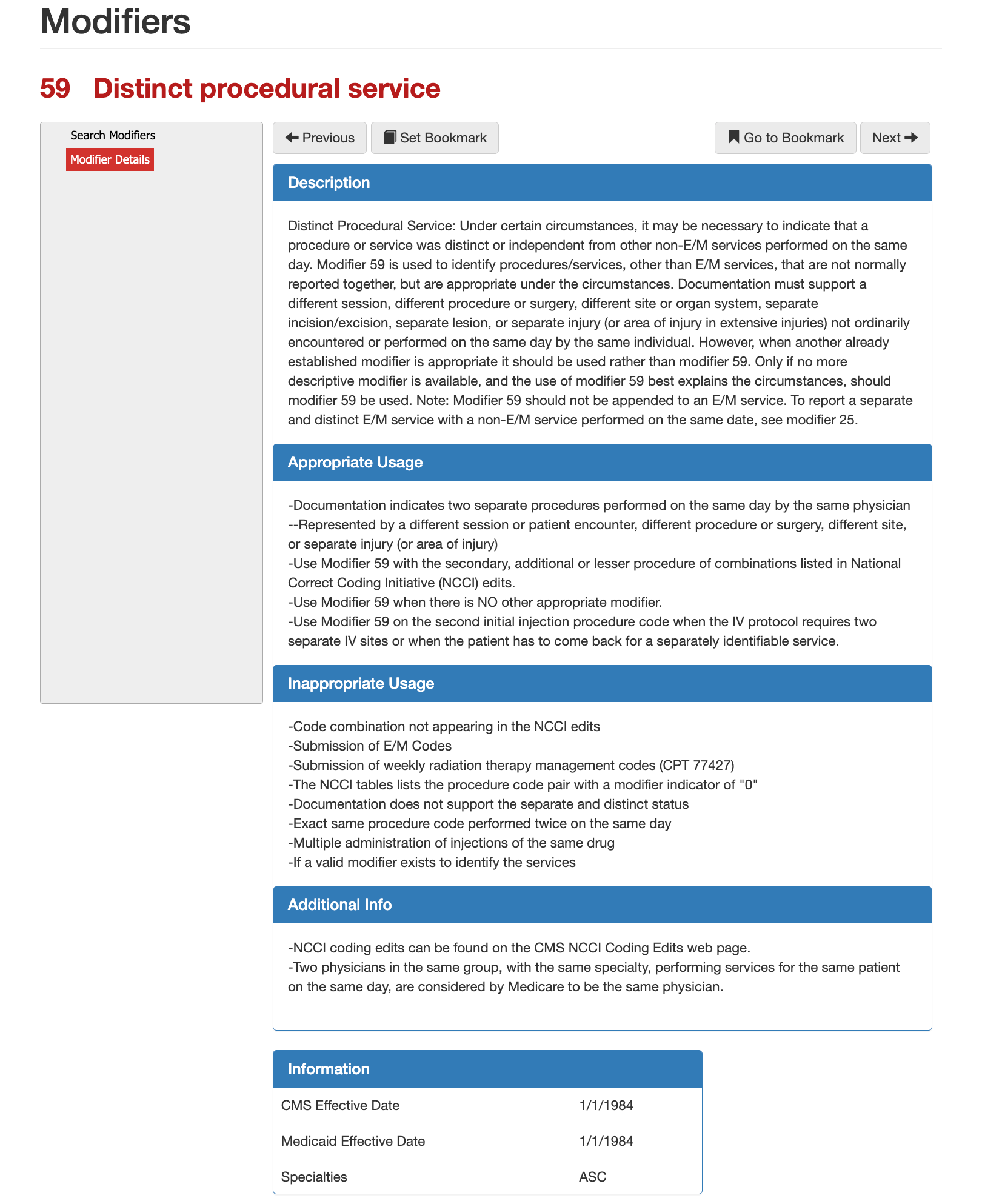
Modifier 59 - Distinct Procedural Service
Modifier 59 is used to indicate that a procedure or service is
separate and distinct from another non-E/M service performed on the same day by the same provider. Its purpose is not to increase reimbursement, but to explain to the payer
why two services that are normally bundled should be considered independent under the circumstances documented. CMS treats modifier 59 as a
last-resort modifier. It should only be used when no other, more specific modifier accurately describes the reason the services are distinct. When applied correctly, modifier 59 allows adjudicators to bypass certain National Correct Coding Initiative (NCCI) edits that would otherwise result in denial.
When is Modifier 59 Appropriate?
Modifier 59 is appropriate when documentation clearly supports that two procedures were performed as separate and independent services. This may include procedures performed during a different session, at a different anatomical site or organ system, through a separate incision or excision, or to treat a separate injury or lesion. It is commonly used on the secondary or lesser procedure when that service would normally be bundled under NCCI edits but is clinically justified as distinct. Modifier 59 may also apply when a patient returns for a separately identifiable service on the same day, such as a second IV injection requiring a different site or a separate encounter. Claims reviewers expect the operative or procedural note to explicitly support the distinct nature of the services. Vague or implied separation is insufficient.
When is Modifier 59 not Appropriate?
Modifier 59 should
not be used when the code combination does not appear in NCCI edits, when the NCCI modifier indicator is “0,” or when another modifier already exists to describe the situation more precisely. It must not be appended to E/M services, weekly radiation therapy management codes, or repeated administrations of the same drug. It is also inappropriate when the
exact same procedure is performed twice on the same day without clear documentation supporting a distinct session or site. Using modifier 59 simply to bypass bundling or force payment is one of the most common compliance red flags identified in audits.
Modifier 59 Relationship to NCCI Edits
Modifier 59 is tightly linked to CMS NCCI coding edits. These edits define which code pairs are normally bundled and whether a modifier may override the edit. When an NCCI modifier indicator allows override, modifier 59 may be used—but only if documentation fully supports the separation. CMS also considers physicians of the same specialty within the same group to be the
same provider for modifier 59 purposes. This means intra-group work does not automatically justify modifier 59 unless the procedural circumstances meet the distinctness criteria.
Modifier 59 Compliance Considerations
From a payer and compliance perspective, modifier 59 is one of the
most heavily scrutinized modifiers. Overuse, inconsistent use, or use without strong documentation frequently results in denials, recoupments, or extrapolated audit findings. Health plans expect modifier 59 usage to be
rare, defensible, and well-documented. Claims systems often flag repeated modifier 59 usage patterns as potential unbundling risk, especially when applied broadly across similar code pairs.
Modifier 59 vs Other Modifiers
Modifier 59 should only be used when no other modifier accurately describes the service. If a distinct E/M service is performed on the same day as a procedure,
modifier 25—not modifier 59—applies. If a more specific X-modifier (XE, XS, XP, XU) explains the separation, CMS prefers those modifiers over 59. Understanding this hierarchy is critical to avoiding denials and maintaining compliance with CMS guidance.
X Modifiers Explained
Why CMS created X Modifiers
The X modifiers were created by CMS to replace broad use of Modifier 59 when a more precise explanation is available. Each X modifier communicates why a service is distinct under National Correct Coding Initiative (NCCI) edits. When documentation clearly supports one of these scenarios, CMS expects an X modifier to be used instead of Modifier 59.
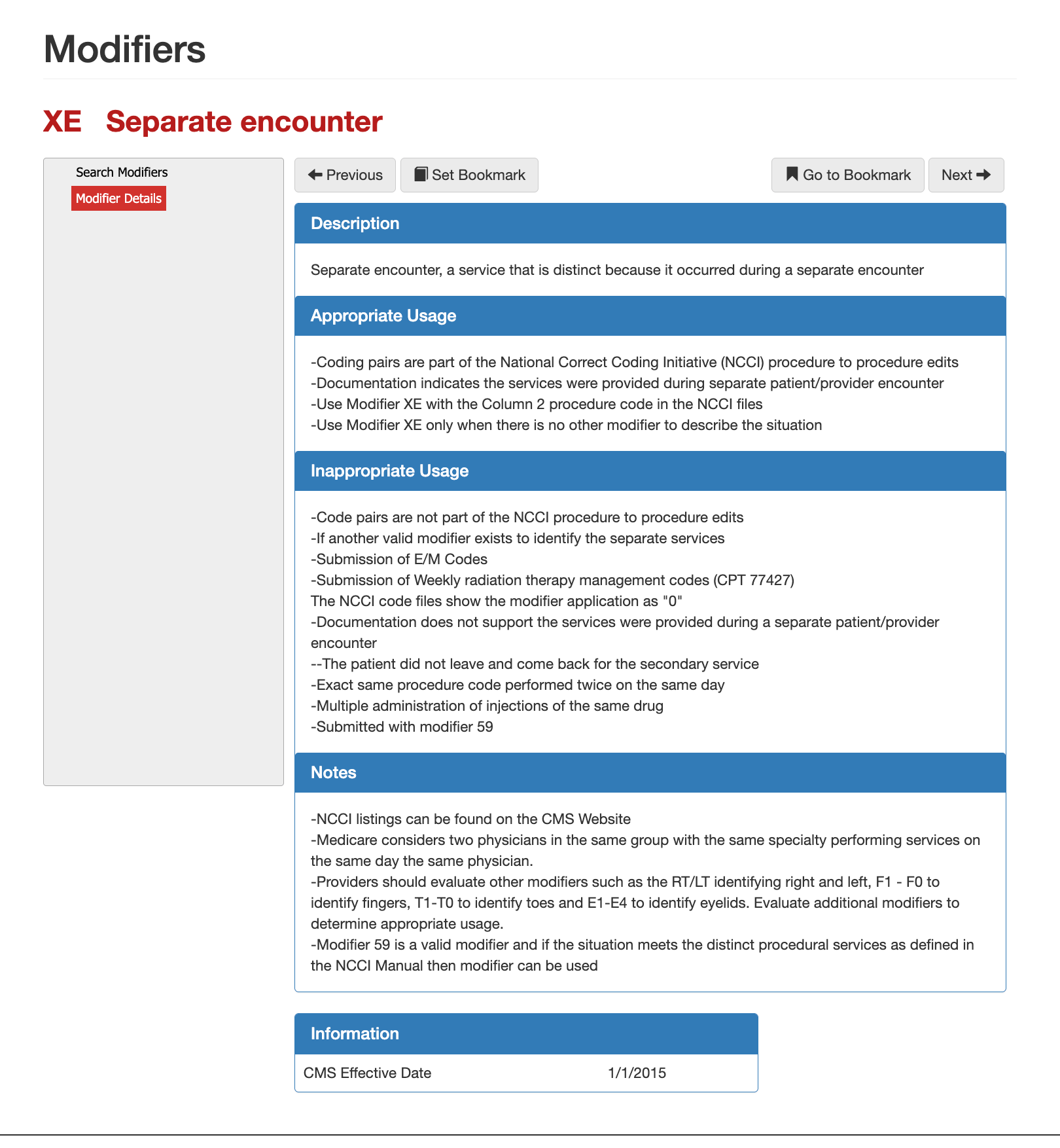
What is Modifier XE?
Modifier XE indicates a service that is distinct because it occurred during a separate patient encounter. This applies when the patient leaves and later returns, or when services are provided at clearly different times that qualify as separate encounters under NCCI guidance.
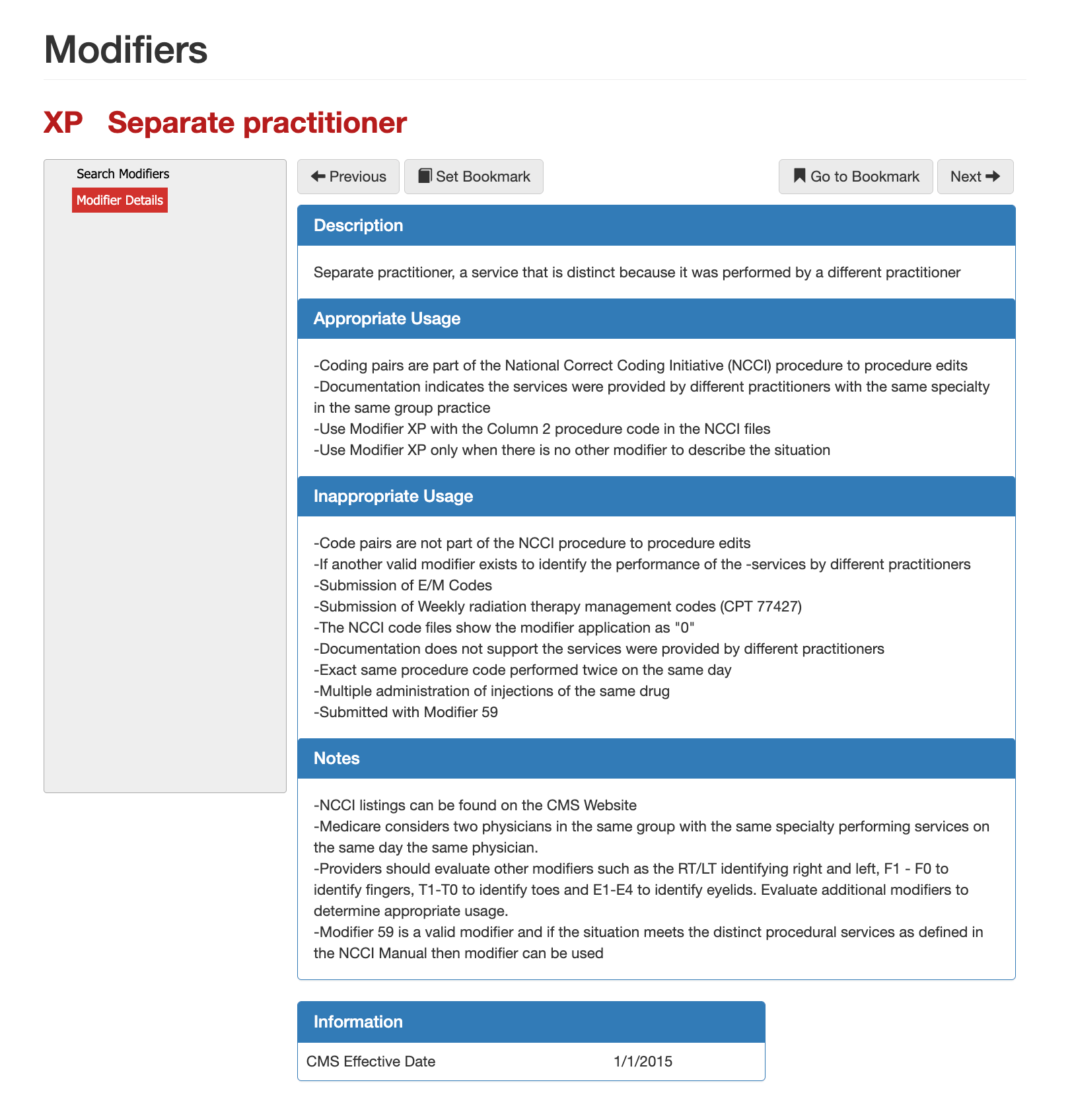
What is Modifier XP?
Modifier XP is used when a service is distinct because it was performed by a different practitioner. CMS considers practitioners of the same specialty within the same group to be the same provider, so documentation must clearly show a different individual practitioner performed the secondary service.
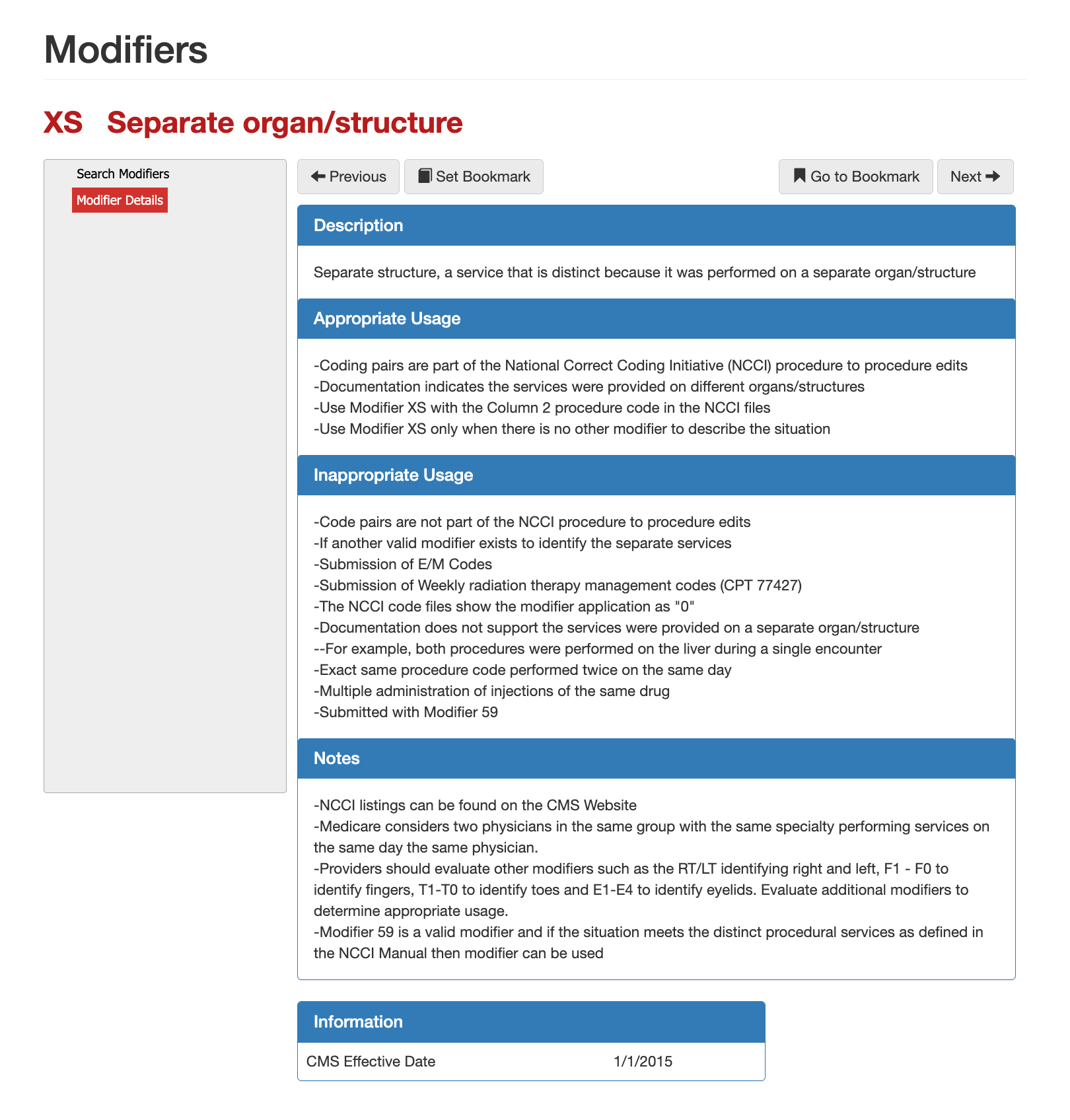
What is Modifier XS?
Modifier XS identifies a service that is distinct because it was performed on a different organ or anatomical structure. The documentation must support that the procedures did not occur on the same organ or structure during the same operative session.
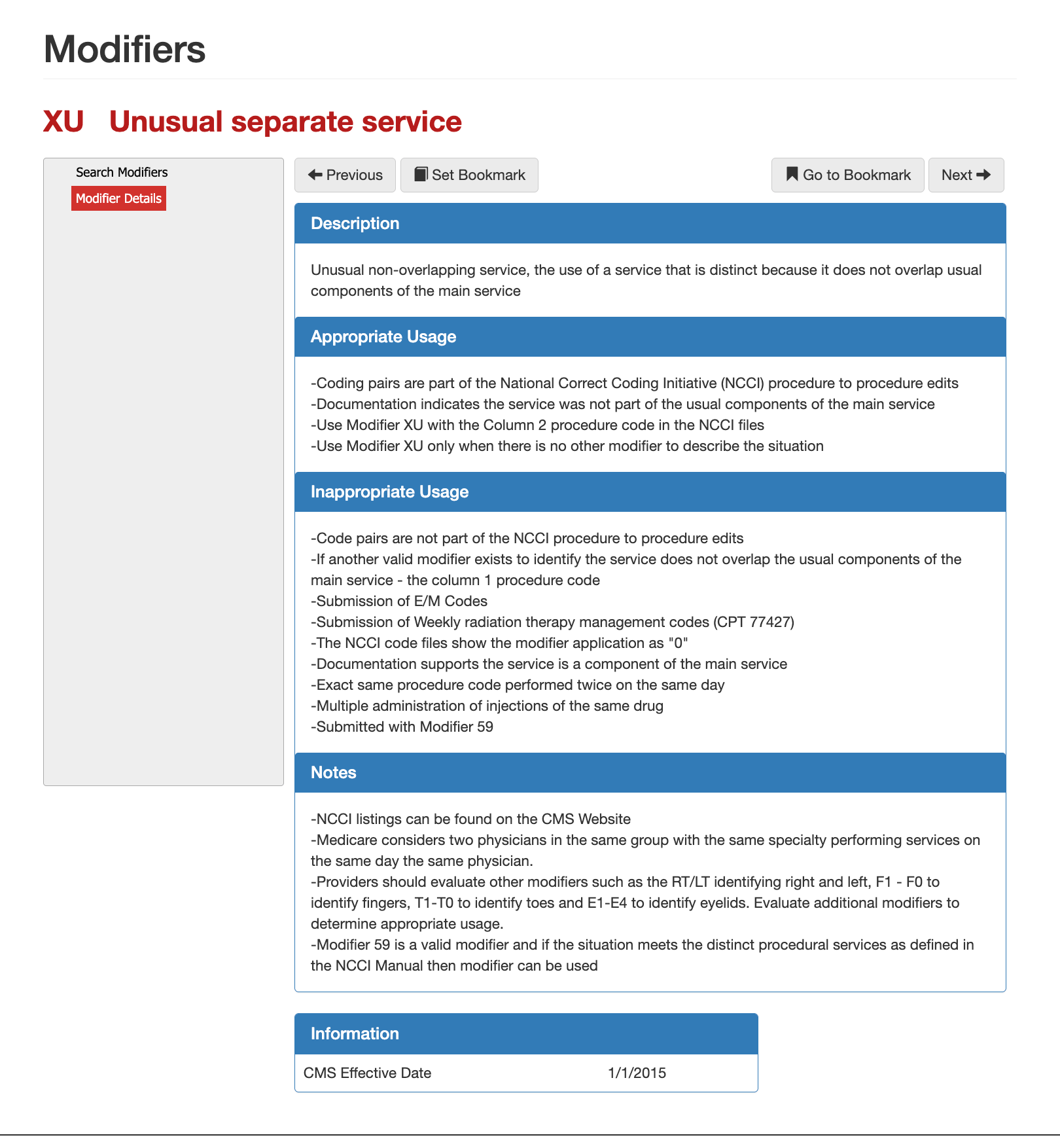
What is Modifier XU?
Modifier XU applies when a service is distinct because it does not overlap the usual components of the primary procedure. This modifier is reserved for uncommon situations where the secondary service is not normally bundled and is not explained by encounter, practitioner, or anatomy alone.
How to choose the right X Modifier?
The correct X modifier depends on why the services are separate, not simply that they occurred on the same date. Modifier XE is appropriate when timing and patient flow create a true separate encounter. Modifier XP should be used only when a different practitioner performed the service and that distinction is clear in the record. Modifier XS is the strongest choice when services are performed on different organs or structures, as it directly addresses anatomical separation. Modifier XU should be used sparingly and only when the service is truly unusual and non-overlapping, and when no other X modifier accurately explains the situation.
CMS guidance is clear that X modifiers should be used
instead of Modifier 59 whenever one applies. Modifier 59 remains valid, but only when none of the X modifiers fully describe the reason the services are distinct. Claims examiners and AI-driven adjudication systems prioritize X modifiers because they reduce ambiguity, improve compliance, and align more closely with NCCI logic.
Summary on Choosing Modifier 51, 59, or X
Choosing between modifier 51, modifier 59, and the X modifiers requires understanding why multiple services appear on the same claim—not simply that they do. Modifier 51 is a payment and sequencing modifier used to apply multiple-procedure pricing when more than one eligible procedure is performed during the same session; it does not establish clinical distinctness. Modifier 59 is a distinct procedural service modifier used only when services that are normally bundled were truly separate and independently reportable, and it should be treated as a last-resort option. The X modifiers (XE, XP, XS, XU) refine modifier 59 by precisely explaining how services were distinct—by encounter, practitioner, anatomy, or non-overlapping service—and are increasingly preferred by CMS, auditors, and automated adjudication systems. From a compliance perspective, the safest and most defensible approach is to use modifier 51 for pricing logic, an X modifier whenever it accurately explains separation under NCCI rules, and modifier 59 only when no more specific modifier applies and documentation clearly supports distinctness.
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others