CPT Code 90837 - Psychotherapy - 60 minutes
90837 cpt code summary
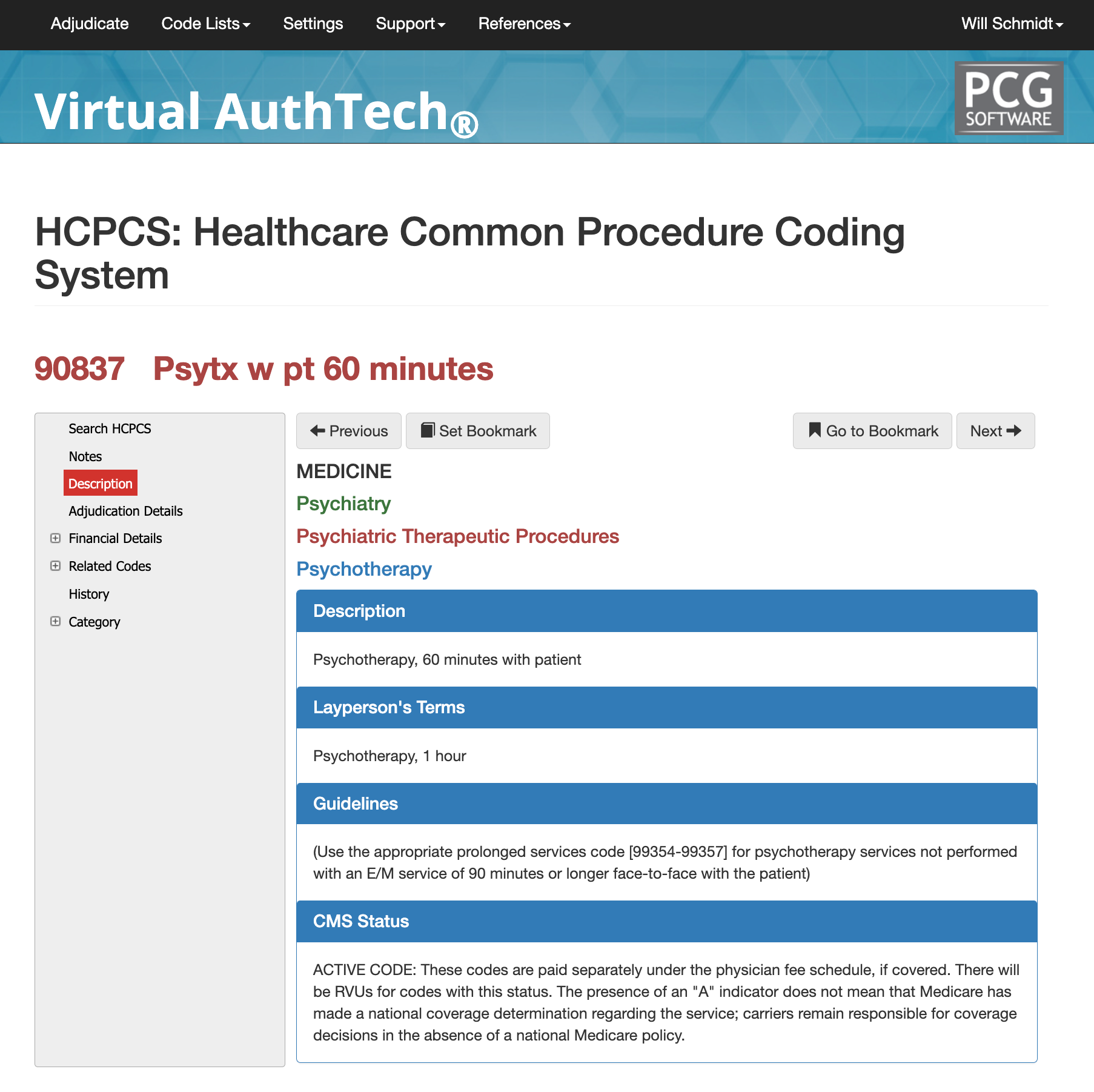
CPT 90837 is the primary code used to report a 60-minute psychotherapy session when the provider spends 53 minutes or more of face-to-face therapeutic time with the patient and/or family member. This code represents an extended psychotherapy encounter that involves insight-oriented therapy, behavioral modification, cognitive interventions, or supportive psychotherapy. Because CPT 90837 is a time-based code, documentation must clearly state total psychotherapy time, therapeutic modality used, and medical necessity for the extended session duration. Many payers scrutinize this code due to its higher reimbursement, making precise documentation essential.
What and when do you use cpt code 90837
What CPT 90837 Represents and When It Should Be Reported
CPT 90837 is reported when the clinician provides at least 53 minutes of psychotherapy within a 60-minute session framework. The service must be primarily psychotherapeutic, meaning the therapist engages the patient in communicative therapeutic techniques aimed at symptom reduction, behavioral change, insight development, or emotional stabilization. The total time reflects direct face-to-face engagement and does not include administrative activities such as charting, scheduling, or late arrivals. This code is most appropriate when the patient’s clinical needs or treatment plan warrant extended time for deeper therapeutic work.
Psychotherapy under 90837 uses communication-based modalities and is not considered medically necessary when the patient cannot meaningfully participate due to cognitive or neurological impairment that prevents therapeutic processing. Clinicians must establish and document the rationale for an extended session rather than a shorter 90834 (45-minute) session, particularly when payer policies limit frequency or duration.
Who bills 90837 most often?
A wide range of behavioral health professionals use CPT 90837, including clinical psychologists, psychiatrists, licensed marriage and family therapists, licensed clinical social workers, licensed professional counselors, psychiatric nurse practitioners, and physician assistants working within the mental health scope. Although psychiatrists may provide psychotherapy with or without E/M services, non-prescribing therapists typically bill 90837 alone. Many commercial and Medicaid plans reimburse 90837 across all independently licensed mental health providers. Medicare reimburses 90837 when performed by clinical psychologists and particular master's-level clinicians based on state eligibility rules.
Proper Documentation for getting 90837 Approved
Psychotherapy codes follow the CPT “time rule.” For 90837, the minimum requirement is
53 minutes of psychotherapy time. If a session falls below 53 minutes, even by one minute, the correct code becomes
90834 (38–52 minutes). Time should reflect uninterrupted therapeutic engagement and must be clearly recorded. Payers often flag or deny 90837 claims when time is missing or ambiguous. Accurate time entry—such as “Psychotherapy time: 58 minutes”—reduces audit risk.
When 90837 May be Reported with an E/M Code
Psychiatrists, nurse practitioners, and physician assistants may report psychotherapy with an E/M code
when both services are provided and separately documented. To bill an E/M on the same date as 90837, the clinician must perform a
significant and separately identifiable evaluation and management service
documented with appropriate medical decision-making, assessment of physical or psychiatric status, prescription management, or coordination of care. Modifier 25 must be applied to the E/M code to indicate that the evaluation was distinct from psychotherapy. Psychotherapy time must exclude time spent on E/M activities.
Interactive Complexity and Add-On Codes
Add-on code 90785 may be reported with 90837 when interactive complexity is present. This involves complicating communication factors, such as family members' involvement in conflict, the use of interpreters, patients with limited expressive ability, or third-party coordination, such as schools or probation departments. The record must demonstrate at least one CPT-defined complicating factor.
Extended sessions beyond the 60-minute psychotherapy duration may allow the use of prolonged service codes in certain circumstances. For example, CPT 99354 may be reported when psychotherapy time exceeds 74 minutes, and 99355 may apply for each additional 30 minutes beyond that threshold. Payers vary significantly in their coverage of prolonged psychotherapy, so clinicians should confirm each payer's policy.
Crisis Psychotherapy Codes vs 90837
CPT 90837 is not used for crisis psychotherapy. When the patient presents in acute crisis, requiring immediate stabilization, extended risk assessment, and complex therapeutic intervention, the correct codes are
90839 (first 60 minutes) and
90840 (each additional 30 minutes). These codes reflect clinical urgency and require documentation of the crisis state, disposition planning, and the time spent addressing the crisis.
Adjudication Details for CPT 90837
Adjudication Details and Claim Characteristics (Virtual AuthTech Data Example)
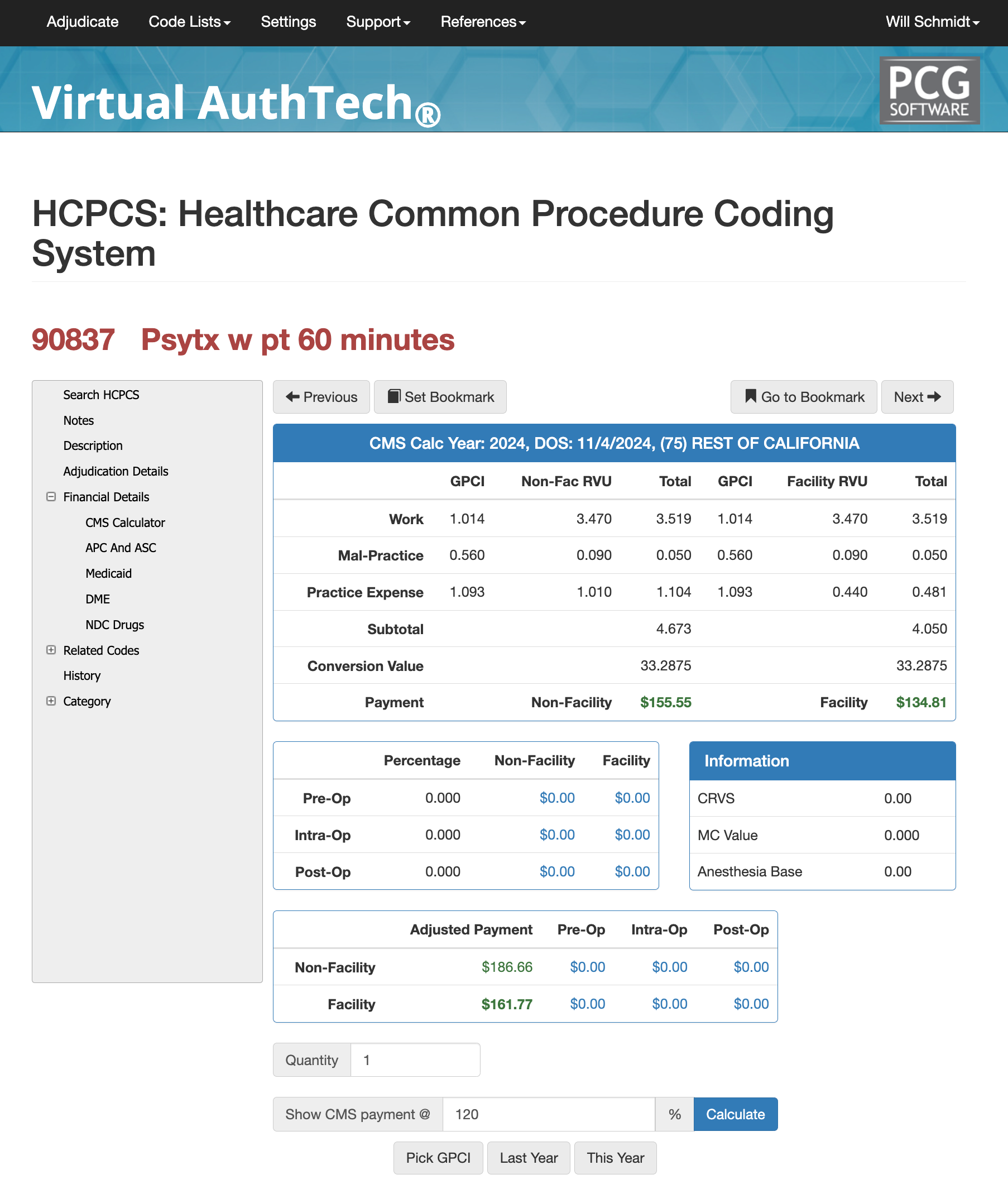
CPT 90837 typically carries zero pre-operative and post-operative global days, is associated with Diagnostic Family 99, and has no age restrictions. Medicare’s Medically Unlikely Edit (MUE) for 90837 is generally low—often 1 or 2 units per date of service—reflecting expectations that extended psychotherapy will not typically occur more than once per day. Payers may impose additional frequency limitations, such as weekly usage caps, based on utilization patterns. Using Virtual AuthTech, payers and providers can model reimbursement using local GPCI values and custom contract percentages to establish rates for extended psychotherapy sessions.
RVU values for 90837 vary by locality but generally include substantial practice expense and work components due to the length and clinical complexity of the service. In California, for example, a non-facility reimbursement rate may exceed $155 depending on local adjustments, while facility-based rates are typically lower.
APC and ASC 90837
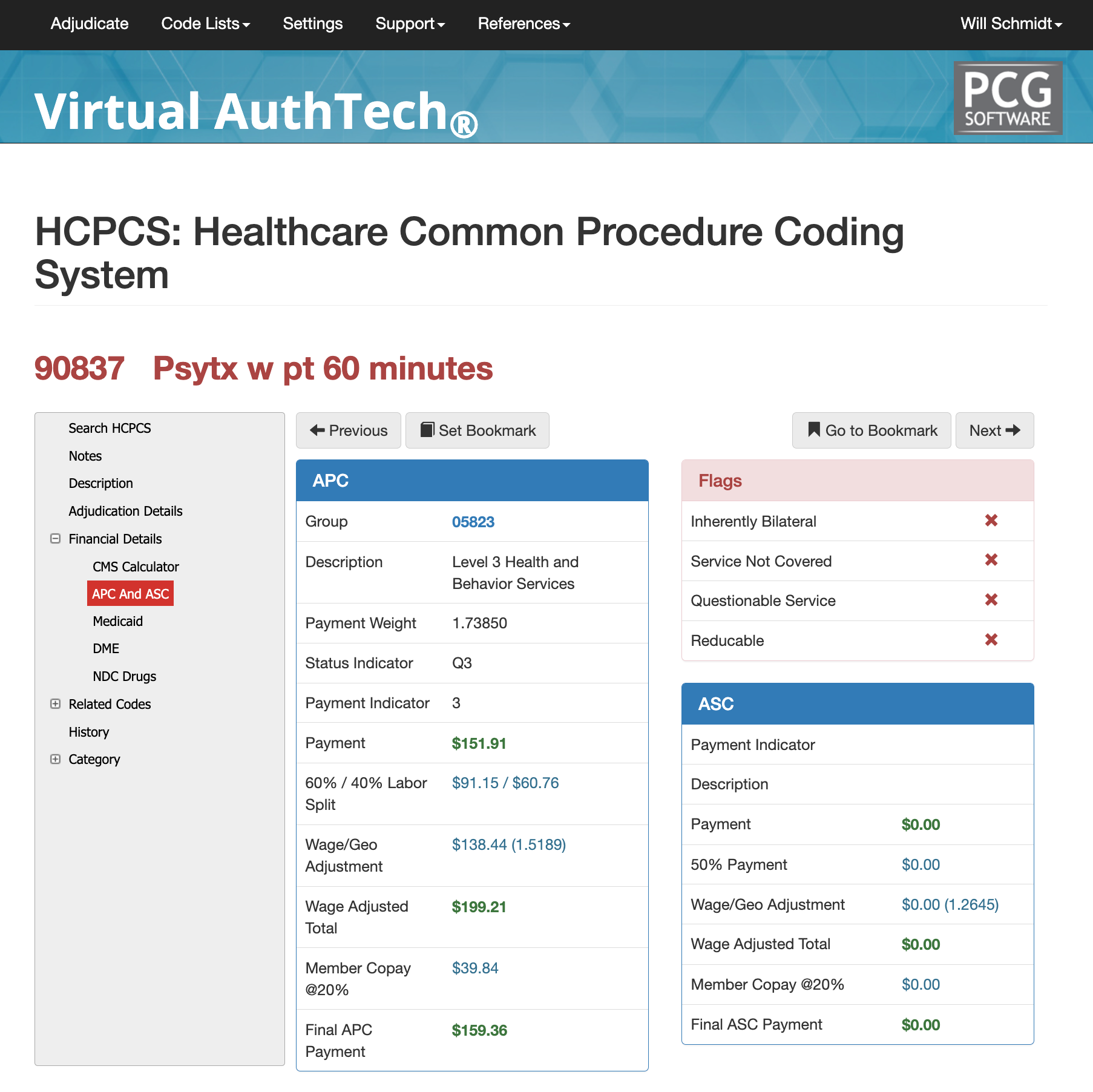
In hospital outpatient settings, 90837 falls within Level 3 Health and Behavior Services, making it subject to bundling under the applicable APC group. Under the ASC payment system, 90837 is not separately reimbursable and is typically packaged as part of the broader encounter. State Medicaid programs vary widely in their reimbursement for 90837, with some requiring prior authorization or imposing strict frequency limits. Providers should verify state-specific rules through Medicaid fee schedules or adjudication modeling tools like Virtual AuthTech.
CCI Bundling and Commond Edit Conflicts with CPT Code 90837
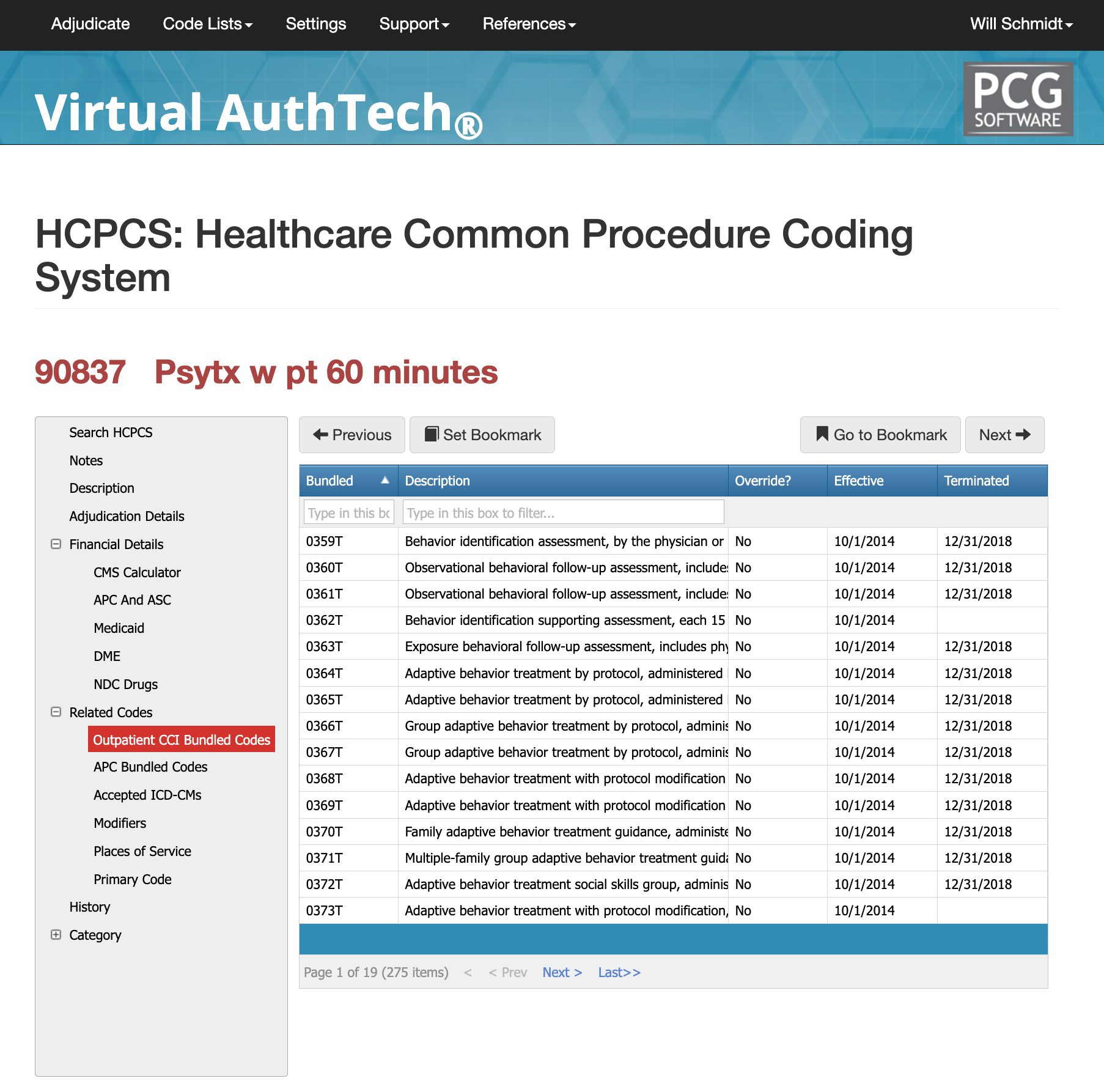
Claims for 90837 often encounter NCCI bundling edits when billed with diagnostic psychiatric evaluations, crisis psychotherapy, psychological testing, or E/M visits lacking modifier 25. Payers may also deny 90837 if documentation appears routine or if time is not explicitly stated. Some private insurers impose internal flags for overuse of extended psychotherapy, triggering medical review. Providers should ensure the psychotherapy note aligns with the documented session duration, therapeutic need, and treatment plan.
Most commonly used modifiers for 90837 CPT Code
The most frequently used modifier for 90837 is
modifier 95, indicating telehealth delivery. Since the COVID-19 public health emergency, many payers have expanded telehealth coverage, but some still require proprietary platforms or specific telehealth codes. Other common modifiers include
HO for master’s-level clinicians,
HP for doctoral-level psychologists, and payer-specific modifiers such as U6, UA, UB, or UC when required for behavioral health reporting. Modifier 25 is used only when psychotherapy is provided in addition to a distinct E/M service by a qualified prescriber.
Places of Service for CPT Code 90837
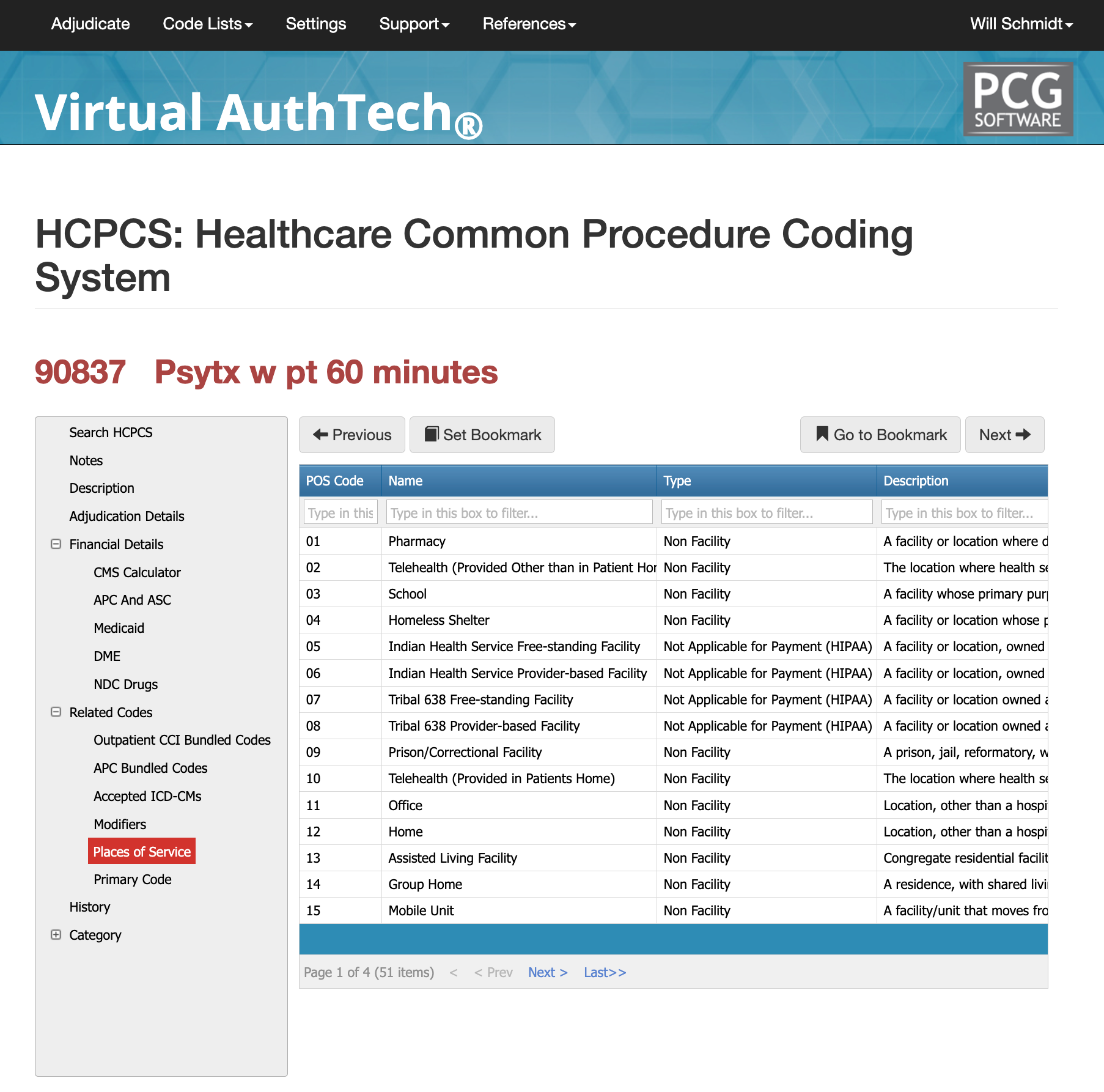
Psychotherapy under 90837 occurs across a variety of clinical settings. The most common include the office (POS 11), telehealth via home or office connection (POS 10 or POS 02), outpatient hospital departments (POS 22 or POS 19), skilled nursing facilities (POS 31), and occasionally emergency departments when psychotherapy is appropriate and medically necessary. The place-of-service code must match the documentation and service delivery method.
Reasons for Denials and FAQs about CPT Code 90837
Most Common Denials for CPT Code 90837
Payers frequently deny 90837 for lack of documented time, absence of medical necessity justification for an extended session, or because the note resembles a routine 45-minute psychotherapy encounter. Other denials occur when the provider attempts to bill more units than allowed by the MUE, when prolonged service codes lack justification, or when interactive complexity is added without supporting factors. Telehealth claims may deny when modifier 95 is omitted or when payer-specific telehealth rules are not followed. Utilizing automated tools such as Virtual Examiner and Virtual AuthTech helps identify documentation gaps and prevent denials before claims are submitted.
FAQs about CPT Code 90837
CPT 90837 is defined as a 60-minute psychotherapy session requiring at least 53 minutes of therapeutic engagement. When sessions are less than 53 minutes, the correct code is 90834. Telehealth delivery is allowed when payer policies permit, typically requiring modifier 95. An E/M service may be billed on the same day as 90837 by psychiatrists or qualified prescribers when a distinct evaluation is performed; modifier 25 must be applied to the E/M code. Prolonged service add-on codes may apply when the psychotherapy session exceeds 74 minutes, subject to payer approval. Prior authorization requirements vary by payer, and some plans limit the frequency of extended psychotherapy sessions.
PCG Software’s Authority and Expertise in CPT Code Interpretation
For more than three decades, PCG Software has supported payers, MSOs, IPAs, TPAs, and clinical organizations in improving behavioral health coding accuracy, preventing fraud and waste, and strengthening medical necessity documentation. Our solutions—including Virtual Examiner®, VEWS™, Virtual AuthTech, and iVECoder®—leverage payer-side adjudication logic to identify coding errors, ensure compliance, and streamline behavioral health claim processing. This resource reflects PCG’s commitment to improving coding literacy, operational efficiency, and financial accuracy across the behavioral health ecosystem.
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others