CPT 20220 defined and usage examples
What will this article about 20220 teach you?
CPT Code 01996 is used to report daily hospital or outpatient follow-up services for patients who have previously received epidural or regional anesthesia. This code captures the evaluation and management work associated with monitoring the patient’s response to the anesthetic injection, assessing pain control, managing side effects, and determining whether additional intervention is necessary. In this article, we break down the AMA and CMS definitions, documentation requirements, common denials, bundled edits, related codes, and financial considerations. You will also learn how AI code scrubbers like Virtual AuthTech and iVECoder reduce errors, ensure compliant billing, and strengthen payment accuracy for anesthesia-related encounters.
The Who, What, When for billing and paying for CPT Code 20220
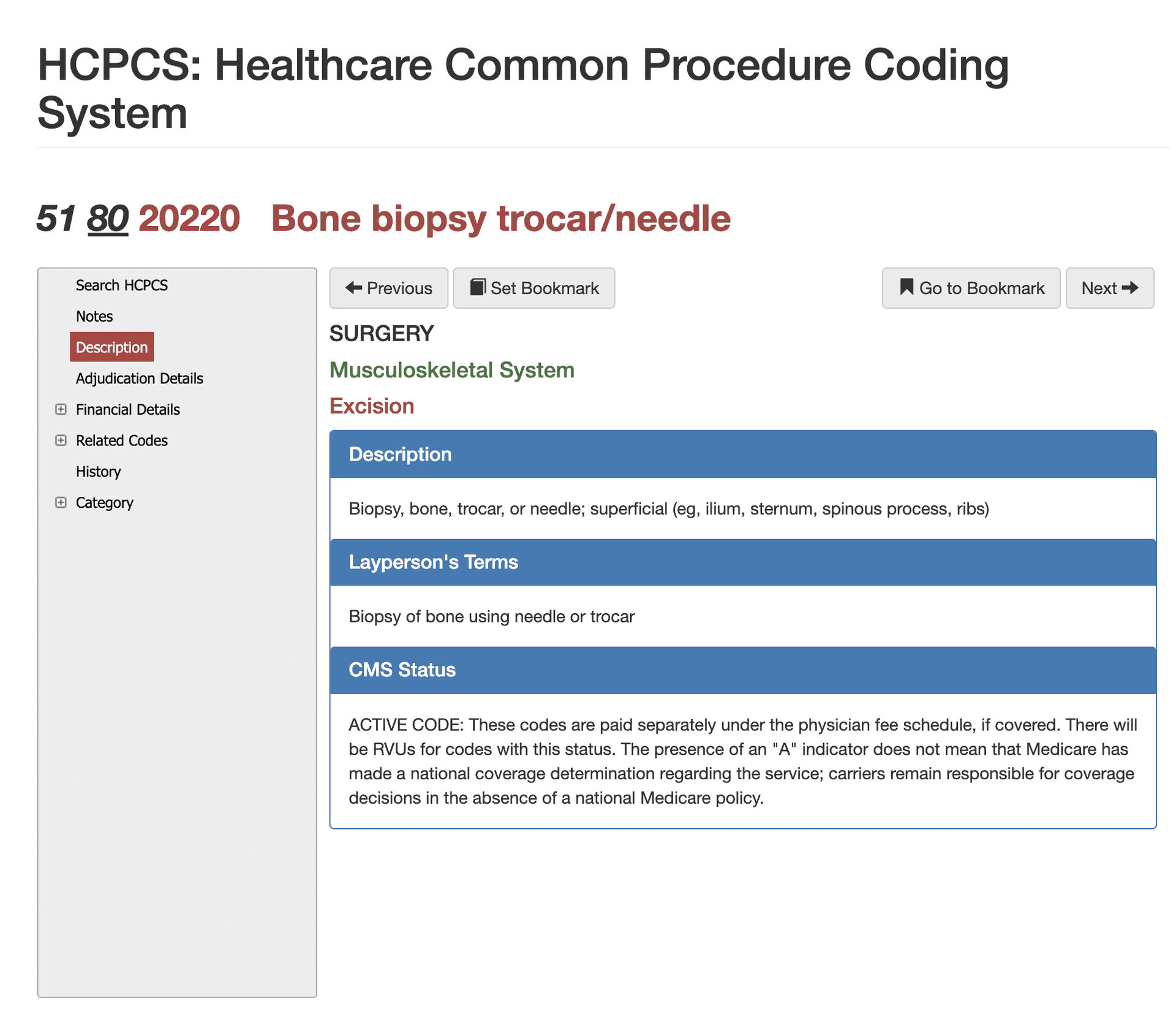
ADefinition of CPT Code 20220 - AMA vs Layperson:
AMA defines CPT 20220 as “biopsy, bone, trocar or needle; superficial.” In simpler terms, this refers to removing a small piece of bone from an area close to the surface using a needle-like device. Providers perform this type of biopsy to confirm or rule out infections, tumors, or metabolic bone disorders. Because it is percutaneous and targets a superficial site, it is less invasive than surgical open biopsies and requires careful distinction from deep bone biopsy procedures.
When is CPT Code 20220 Used?
CPT 20220 represents a percutaneous biopsy of a superficial bone site, meaning the bone can be accessed without cutting through deep layers of muscle or complex anatomical structures. The procedure typically involves inserting a needle or trocar through soft tissue to obtain a bone sample for pathology review. Clinicians rely on this test when imaging raises concern for infection, neoplasm, unexplained lesions, osteopenic changes, or complications related to orthopedic implants. Because bone biopsies carry clinical risk, documentation must clearly justify why sampling was necessary and how the results will guide treatment. Claims examiners look for precise site identification, confirmation that the biopsy was superficial, and evidence that the service met medical necessity criteria.
Who bills for CPT Code 20220?
A wide range of specialists may bill CPT 20220, especially those who routinely treat bone and joint conditions. Orthopedic surgeons frequently perform superficial biopsies to evaluate abnormalities before surgical planning. Interventional radiologists also perform many of these biopsies under image guidance, particularly when the lesion requires precise targeting. General surgeons, infectious disease physicians, and pain specialists may request or perform this biopsy when bone infection or metabolic disease is suspected. In facilities where scope-of-practice laws allow it, nurse practitioners and physician assistants may perform superficial biopsies under physician supervision. Because many of these procedures occur in outpatient hospital or ASC settings, both professional and technical components may appear on claims.
Top Diagnosis ICD-10 for CPT 20220
Diagnosis codes must clearly support the need for a bone biopsy. Common ICD-10 pairings include:
- M86.0–M86.9 – Osteomyelitis
- C40–C41 – Bone tumors
- M85.8 – Other bone lesions
- M89.9 – Bone disorder, unspecified
- M90.x – Metabolic bone disease
- T84.x – Complications of orthopedic implants
Vague pain diagnoses alone (e.g., M79.6) rarely justify a bone biopsy. Medical necessity must be explicit.
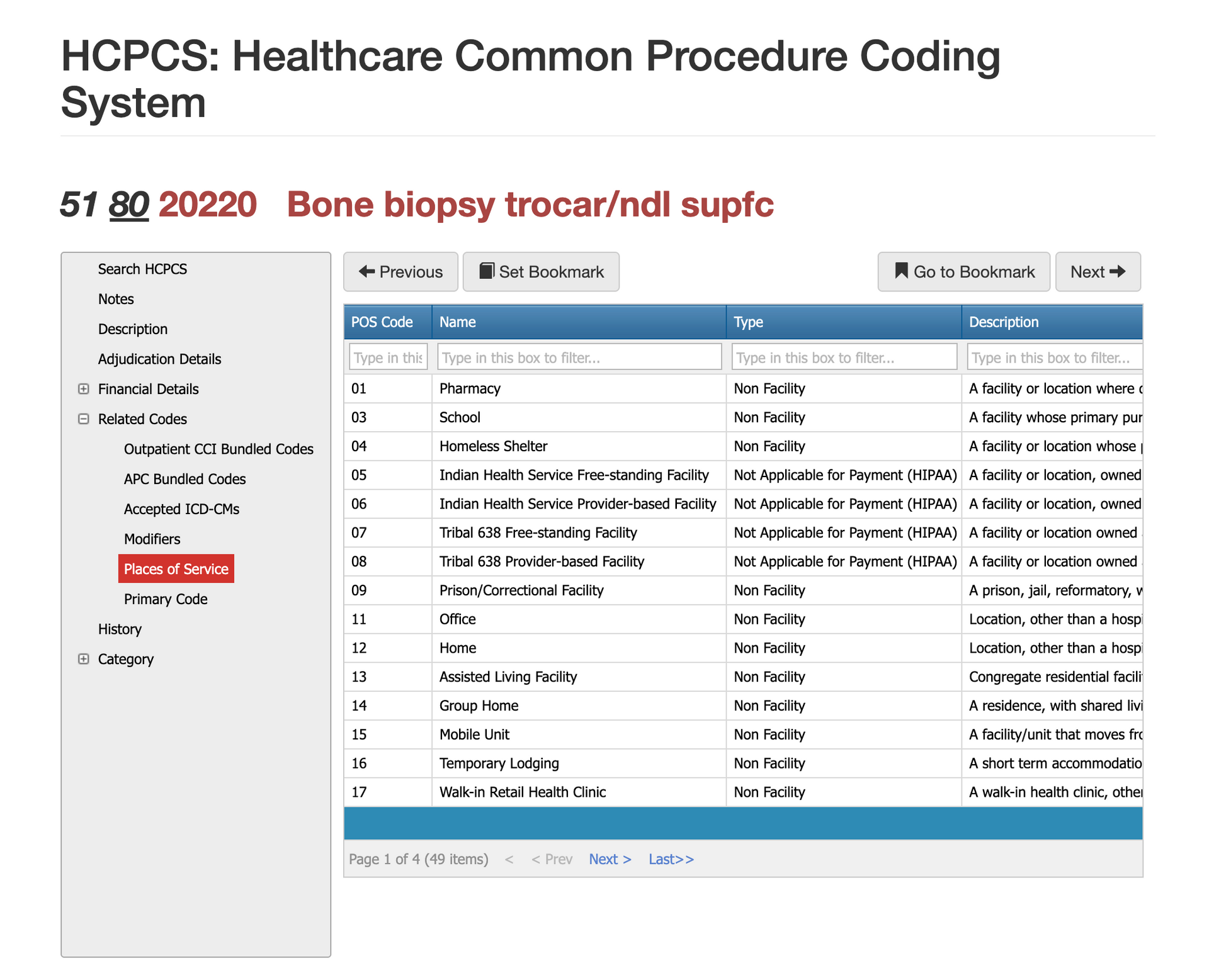
Places of Service for CPT Code 20220
The most common POS codes for CPT 20220 include:
- 22 – Hospital outpatient
- 24 – Ambulatory surgical center
- 11 – Physician office (when performed in-office with proper equipment)
- 21 – Hospital inpatient for medically complex or infectious scenarios
- 23 – Emergency department (less common but possible)
The POS must reflect where the biopsy occurred—not where the patient was evaluated.
Incorrect POS is a top-five denial reason for this code.
Proper Documentation for CPT Code 20220
Accurate and thorough documentation is essential for preventing denials and for distinguishing CPT 20220 from other musculoskeletal biopsy codes. The procedure note must identify the specific bone being sampled and describe why the biopsy was medically necessary, such as concern for infection, malignancy, or unexplained bone lesions. Providers should document the technique used, including the needle or trocar size, the number of passes, and whether imaging guidance assisted the procedure. The record should also clarify that the access was superficial and did not involve deep tissue dissection, as this determines whether 20220 or 20225 applies. Pathology submission details and any immediate complications must be included to complete the record.
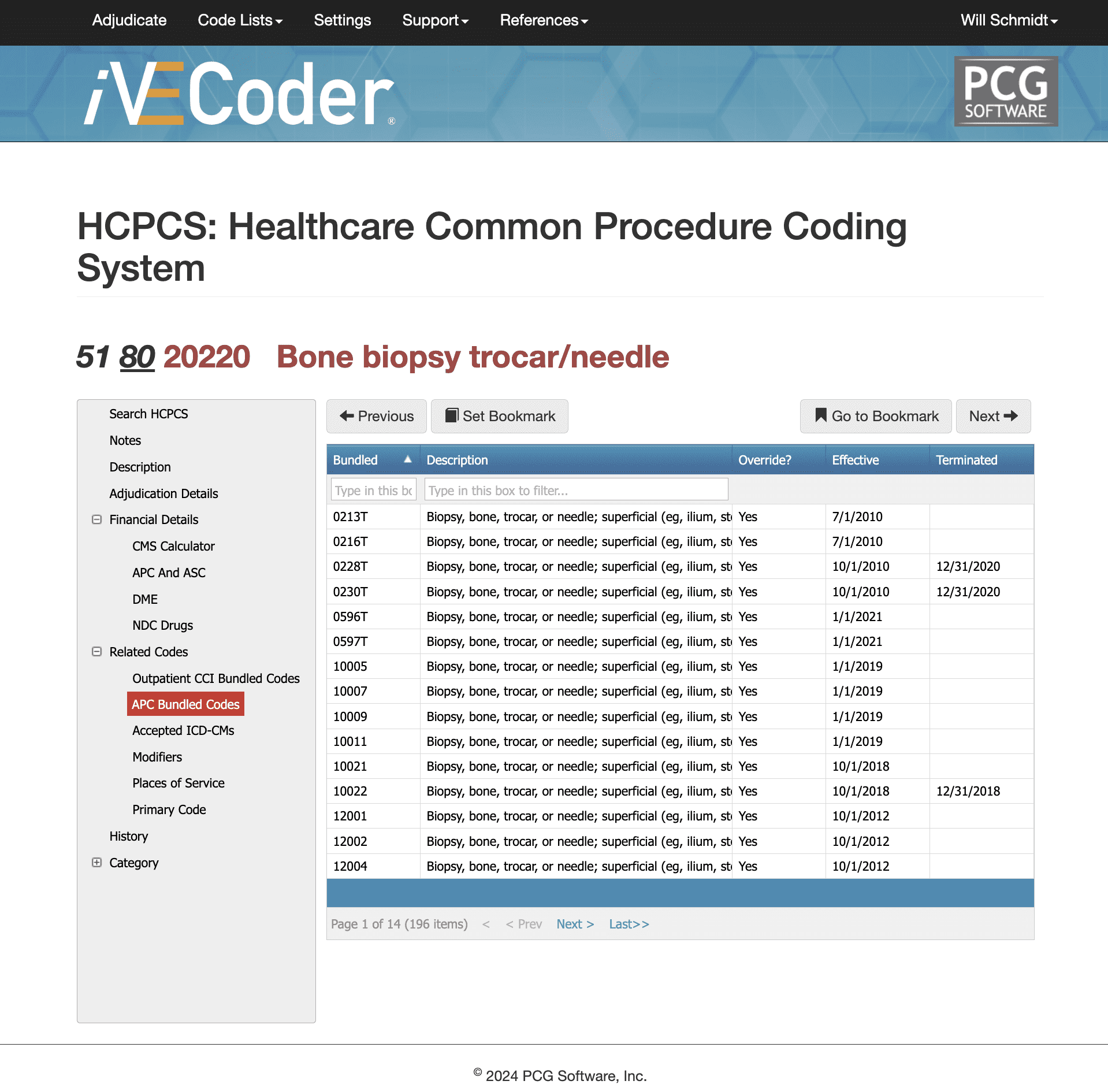
Bundled Codes for CPT Code 20220
Superficial bone biopsy interacts with several bundling rules across outpatient and facility payment systems. Under CCI edits, 20220 may bundle with codes for imaging guidance, debridement, incision procedures, or broader musculoskeletal surgeries performed on the same date. When imaging guidance is used, the corresponding add-on code must be properly documented to avoid denials for incorrect unbundling. In OPPS settings, CPT 20220 typically falls within APC groups that package ancillary services, meaning imaging or minor supportive procedures may not be separately reimbursed. ASCs may also package 20220 into the payment for a primary orthopedic procedure when the biopsy is part of the surgical workflow. Virtual Examiner is often used to verify bundling status, detect unintentional unbundling, and ensure the claim meets CMS payment integrity rules.
Related CPT Codes for 20220
CPT 20220 sits within a family of musculoskeletal biopsy codes that differ primarily by the depth of access, technique, and anatomical complexity. CPT 20225, which represents a deep bone biopsy, is used when the provider must dissect through deeper tissues or when the bone site is not readily accessible by superficial approach. Open surgical biopsy codes in the 20100 series apply when bone must be surgically exposed rather than accessed percutaneously. Imaging guidance codes may also be used when radiologic assistance is documented. Understanding these distinctions is essential because incorrect code selection can lead to significant overpayment or underpayment.
| CPT Code | Descriptor | How It Differs From 20220 | Time Requirement | Key Difference |
|---|---|---|---|---|
| 20220 | Bone biopsy, trocar or needle; superficial | Used for percutaneous biopsy of superficial bone without deep dissection. | 10–19 min | Very limited problems; low complexity |
| 20225 | Bone biopsy, trocar or needle; deep | Requires deeper access through muscle or complex anatomy. Most common alternative to 20220 when depth is unclear. | 20–29 min | Routine, stable conditions; minimal risk |
| 20100 | Exploration of wound; superficial | Not a biopsy. Used for wound exploration or foreign body evaluation. Should not replace 20220. | 30–39 min | Multiple conditions, medication changes, test interpretation |
| 20103 | Exploration of wound; deep | Procedural exploration, not tissue sampling. Incorrect when diagnosis requires pathology. | 40–54 min | Severe issues, significant data review, high-risk decisions |
| 20206 | Needle biopsy, muscle | Soft-tissue only. Used when sampling muscle rather than bone—commonly mis-coded. | ||
| 20207 | Biopsy, muscle, deep | Similar in concept to 20206, but requires deeper access. Not a bone service. | ||
| 20900 | Bone graft, minor | Surgical service for graft harvest—not diagnostic biopsy. | ||
| 77012 | CT guidance for biopsy | Add-on to 20220 when imaging guidance is used; should not be billed alone. | ||
| 77002 | Fluoroscopic guidance | Add-on code when fluoroscopic guidance assists bone biopsy. | ||
| 88305 | Pathology, Level IV | Lab code billed by the pathologist after tissue is obtained. Often paired with 20220. | ||
| 88311 | Decalcification procedures | Used when bone tissue requires decalcification before microscopic evaluation. |
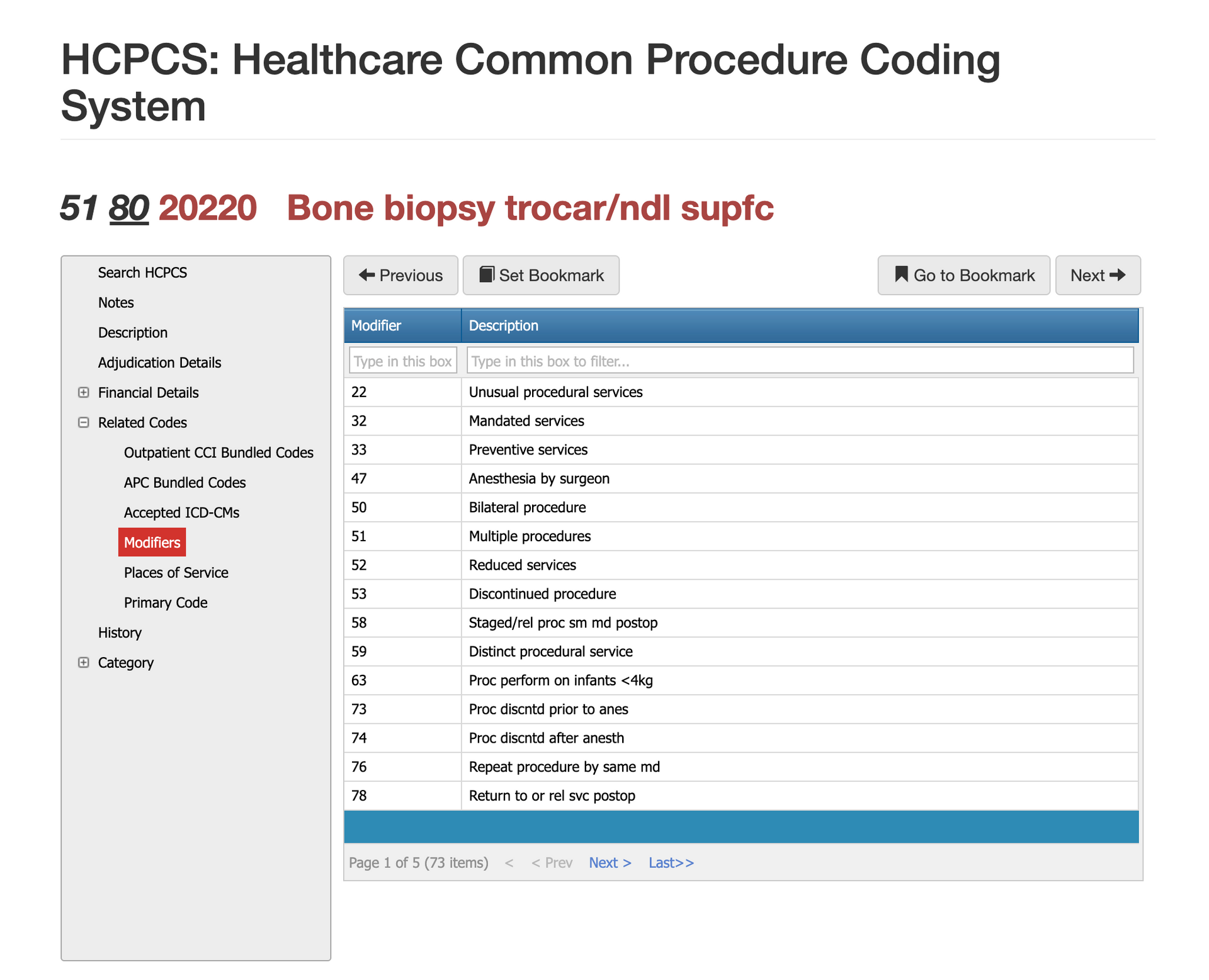
Modifier Guidance for CPT Code 20220
Several modifiers apply to bone biopsy claims depending on the circumstances. Modifier 26 identifies the professional component when the provider interprets results without furnishing the equipment or staff used for the technical component. Modifier TC applies when the facility provides the technical service without billing the professional component. When a biopsy is performed in conjunction with other unrelated procedures, modifier 59 may be necessary to indicate that the service was distinct and separately reportable. Anatomical modifiers such as RT and LT help clarify laterality when bone samples are taken from one side of the body. Claims may suspend or deny when modifiers do not align with documentation, so their use must be precise.
Modifier 26 for CPT Code 20220
Modifier 26 is used when the clinician provides only the professional interpretation of the biopsy procedure or imaging guidance while another entity bills the technical component. This is common when radiologists interpret image-guided biopsies performed in hospital outpatient settings. Claims examiners expect documentation showing the physician’s review, supervision, and interpretation rather than ownership of equipment or staff.
Modifier TC for CPT Code 20220
Modifier TC is applied when a facility supplies the equipment, staff, and resources to perform the technical portion of the biopsy, but the interpreting provider bills separately. This modifier is frequently used in hospital outpatient departments, freestanding imaging centers, or orthopedic facilities. TC billing must align with POS coding, as mismatches between professional-only and technical-only claims often trigger payment holds.
Modifier 59 for CPT Code 01996
Modifier 59 is used when the superficial bone biopsy is separate and distinct from another procedure performed on the same day. This may apply when the biopsy is taken from a different anatomical site or when it is clinically independent of the primary service. Examiners look for clear documentation that the biopsy was not an integral or bundled part of another musculoskeletal procedure.
Modifier RT/LT for CPT Code 20220
Right (RT) and Left (LT) modifiers help clarify which anatomical side was sampled during the procedure. They are essential when a biopsy is performed on paired bones or when future procedures may differ by side. Missing laterality is one of the most common reasons payers suspend biopsy claims for manual review.
Modifier 51 for CPT Code 20220
Modifier 51 is used when CPT 20220 is performed alongside other surgical or procedural services during the same encounter. Because secondary procedures typically reimburse at a reduced rate, payers use modifier 51 to adjust payment accordingly. Documentation must show that the biopsy required additional work beyond the primary procedure.
Most Common Reasons for 20220 CPT Denials
Superficial bone biopsy claims are denied most often when documentation does not clearly distinguish superficial from deep access, when the diagnosis does not justify invasive sampling, or when bundling rules are not followed. Because this procedure often overlaps with imaging guidance, pathology services, and broader musculoskeletal interventions, payers scrutinize these claims closely to ensure medical necessity and correct code selection.
Missing or Insufficient Documentation - "Superficial"
One of the most common denials occurs when the operative note does not explicitly describe that the biopsy site was superficial. If depth is unclear, examiners default to assuming the work may fit deeper biopsy code 20225 or that documentation is insufficient for either. Clear statements about tissue layers traversed, technique used, and accessibility of the bone eliminate this issue.
Diagnosis Does Not Support Biopsy Medical Necessity
Payers frequently deny CPT 20220 when the diagnosis reflects nonspecific pain, swelling, or vague abnormalities without explanation of why a tissue sample was required. ICD-10 must correlate with an indication such as suspected infection, tumor, metabolic bone disease, or unexplained imaging findings. Tying the biopsy decision directly to the diagnostic concern prevents most medical-necessity denials.
Bundling Conflicts or Incorrect Use of Imaging Guidance Codes
Claims are often denied when imaging guidance is billed but not documented, or when the biopsy overlaps with procedures that bundle under CCI edits. Radiologic assistance must include a documented physician role, images saved to the record, and a clear statement of guidance. Unintentional unbundling with musculoskeletal procedures or debridement also results in denials and later audits.
Diagnosis Does Not Support Biopsy Medical Necessity
Payers frequently deny CPT 20220 when the diagnosis reflects nonspecific pain, swelling, or vague abnormalities without explanation of why a tissue sample was required. ICD-10 must correlate with an indication such as suspected infection, tumor, metabolic bone disease, or unexplained imaging findings. Tying the biopsy decision directly to the diagnostic concern prevents most medical-necessity denials.
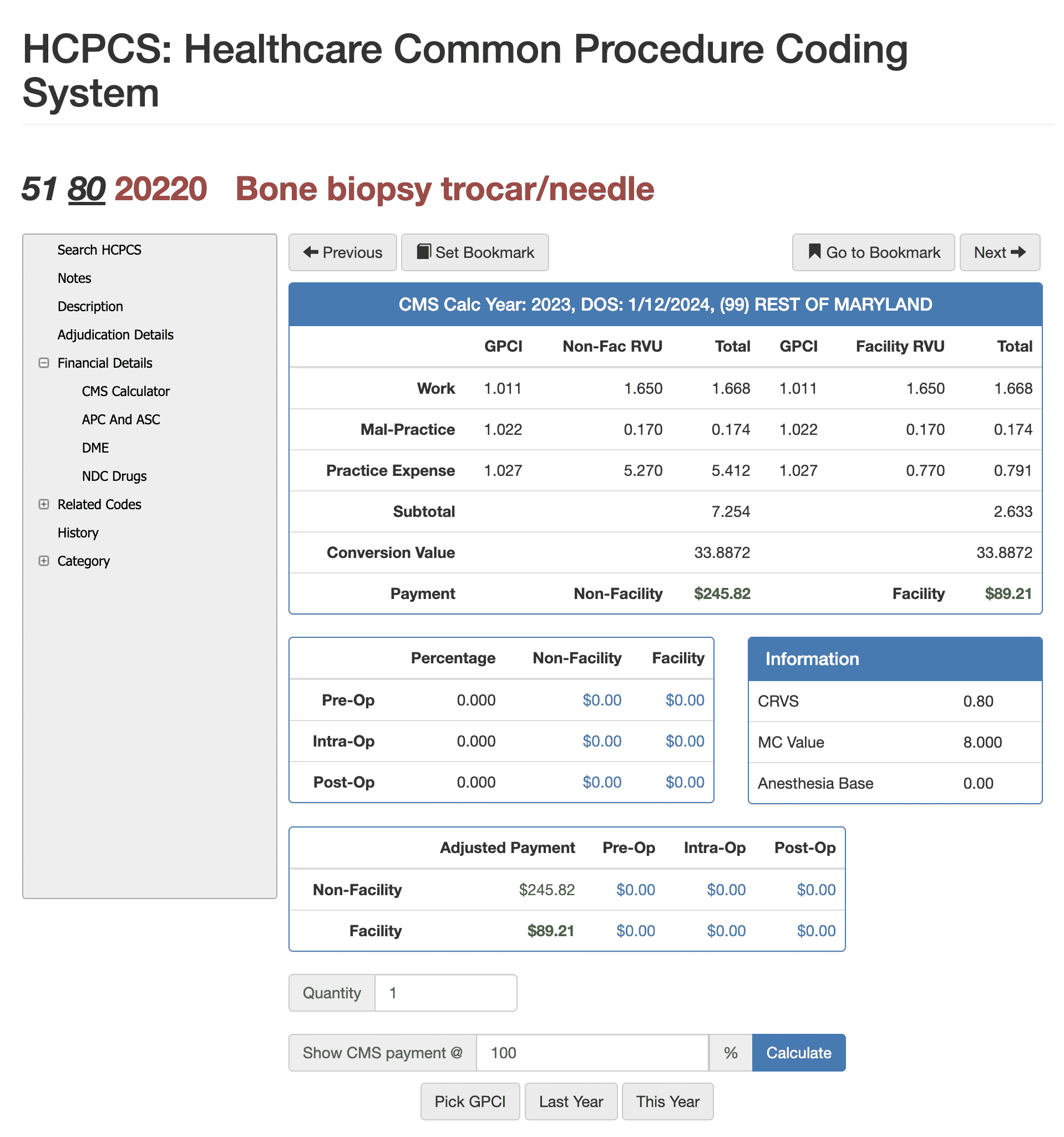
RVUs and Financials for CPT Code 20220
RVU Negotiation Guide for CPT 20220
Reimbursement for CPT 20220 depends on its RVU structure, which includes work RVUs, practice expense RVUs, and malpractice RVUs adjusted through the Geographic Practice Cost Index. Because bone biopsies involve procedural skill and pathology handling, the code carries higher relative value compared to evaluation and management visits. Using Virtual AuthTech on the payer side or iVECoder on the provider side makes it possible to evaluate how reimbursement shifts when different Medicare percentages or geographic adjustments apply. These tools allow users to model payment at 100% of Medicare or alternative contract percentages, compare facility and non-facility rates, and analyze out-of-network pricing. Both payers and providers use these simulations to negotiate fair, compliant rates and ensure that compensation aligns with the complexity of diagnostic bone biopsy work in different regions.
The Easier Way to Research codes
For more than 30 years, PCG Software has supported Health Plans, MSOs, IPAs, TPAs, and provider organizations in improving coding accuracy, strengthening compliance, and reducing fraud, waste, and abuse. Our solutions, including Virtual Examiner®, VEWS™, and iVECoder®, are built on decades of payer-side adjudication experience and reflect the same logic used by health plans nationwide. National regulatory guidance, payer policies, compliance standards, and large-scale claims review patterns inform this CPT 69210 analysis.
Toss out the CPT book.
Stop researching articles.
Sign up for iVECoder today!
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others