CPT 11104 - Tangenital Skin Biopsy Guide
Quick Summary for CPT Code 11104
CPT
11104 describes a
tangential skin biopsy of a single lesion, performed with instruments such as a scalpel, shave tool, or dermablade. This code is used when the clinician removes a superficial portion of skin for diagnostic evaluation and submits the specimen for pathology review. Because 11104 represents a procedural service rather than a simple evaluation, payers scrutinize documentation closely—especially around technique, lesion description, clinical suspicion, and the medical necessity for biopsy. This guide explains when 11104 is appropriate, who bills it, how claims examiners evaluate supporting notes, and what documentation prevents denials and downcoding.
The Who, What, When for billing and paying for CPT Code 11104
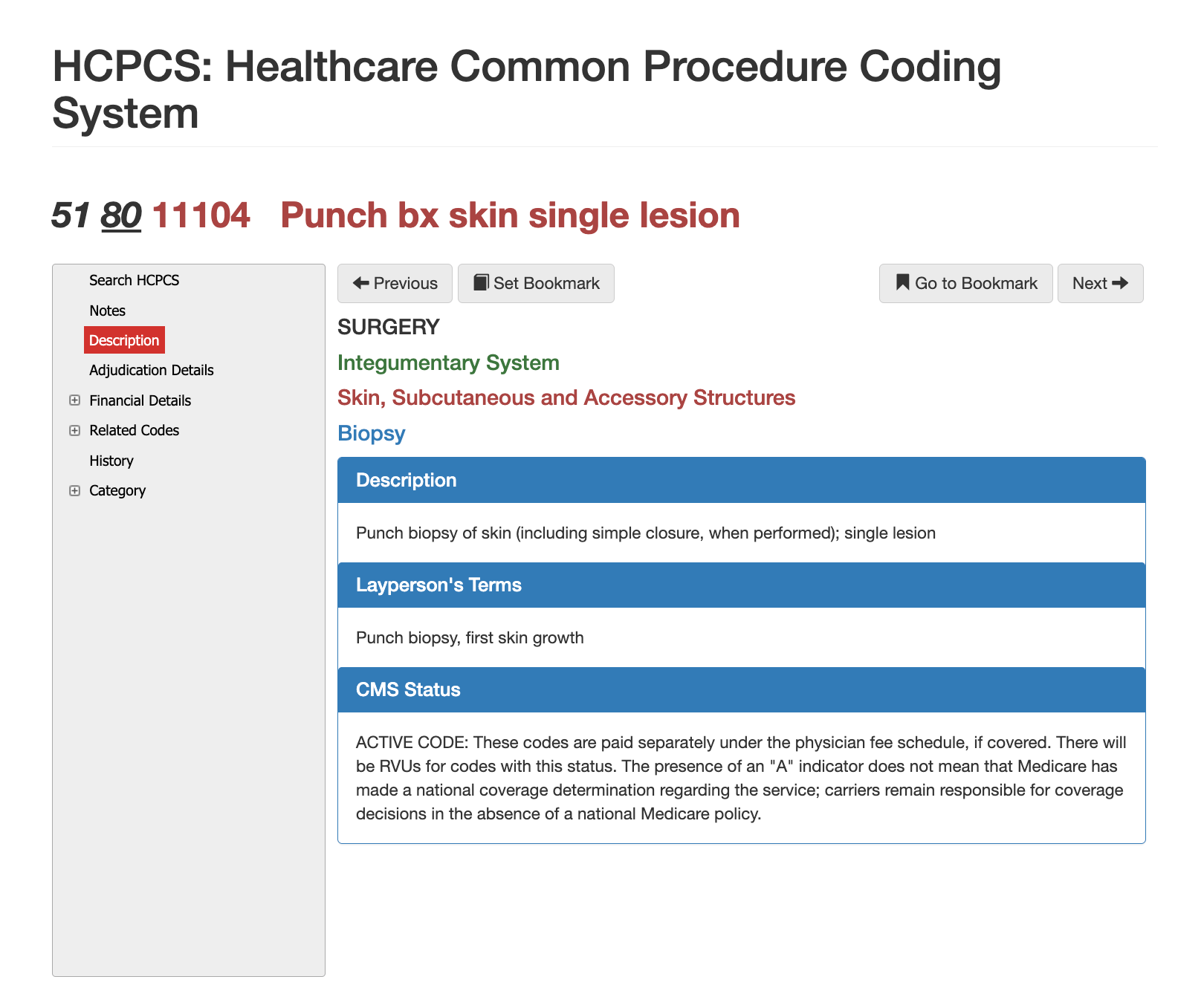
Definition of CPT Code 11104 - AMA vs Layperson:
The AMA defines
11104 as a
tangential biopsy of skin using tools that remove a sample through a horizontal slicing motion. The specimen is collected for histopathologic analysis, and the code refers to a
single lesion, with add-on codes used for additional lesions. In layperson terms, 11104 is used when a doctor takes a surface-level skin sample to determine whether a rash, growth, or spot is benign, cancerous, or indicative of another disease. It is not a full excision. It is not a punch biopsy. It is a shallow diagnostic sampling technique.
When is CPT Code 11104 Used?
11104 is reported when a clinician performs a tangential biopsy for diagnostic purposes. This typically occurs when a patient presents with a lesion of unknown behavior, a changing mole, persistent dermatitis, non-healing skin abnormalities, or potential malignancy. The technique involves superficial sampling rather than deep tissue removal, making it appropriate for lesions where the goal is to obtain sufficient tissue for microscopic review without performing a full excision.
Claims reviewers confirm that the documentation describes:
- The lesion and clinical concern
- The tangential technique used
- The location and size
- The tissue sample was sent to pathology
If these elements are missing, payers frequently deny or recode the service.
Who bills for CPT Code 11104?
Dermatologists represent the largest group of providers billing 11104, followed by family physicians, general surgeons, plastic surgeons, wound care specialists, and urgent care clinicians. Nurse practitioners and physician assistants also perform tangential biopsies when supported by scope of practice and payer policies. Because biopsies generate both professional and pathology claims, payer systems often cross-check procedural notes against pathology billing patterns to ensure clinical and documentation consistency.
Top Diagnosis ICD-10 for CPT 11104
A range of diagnoses support the medical necessity for a tangential biopsy. Common examples include skin lesions of uncertain behavior, actinic keratoses, suspicious moles, dermatologic eruptions unresponsive to treatment, chronic rashes, pustular eruptions, and neoplastic conditions requiring confirmation. Claims examiners look for clear alignment between the diagnosis and the need to obtain tissue for microscopic analysis. When documentation suggests a purely cosmetic reason or a routine preventive exam, payers frequently deny 11104 as not medically necessary.
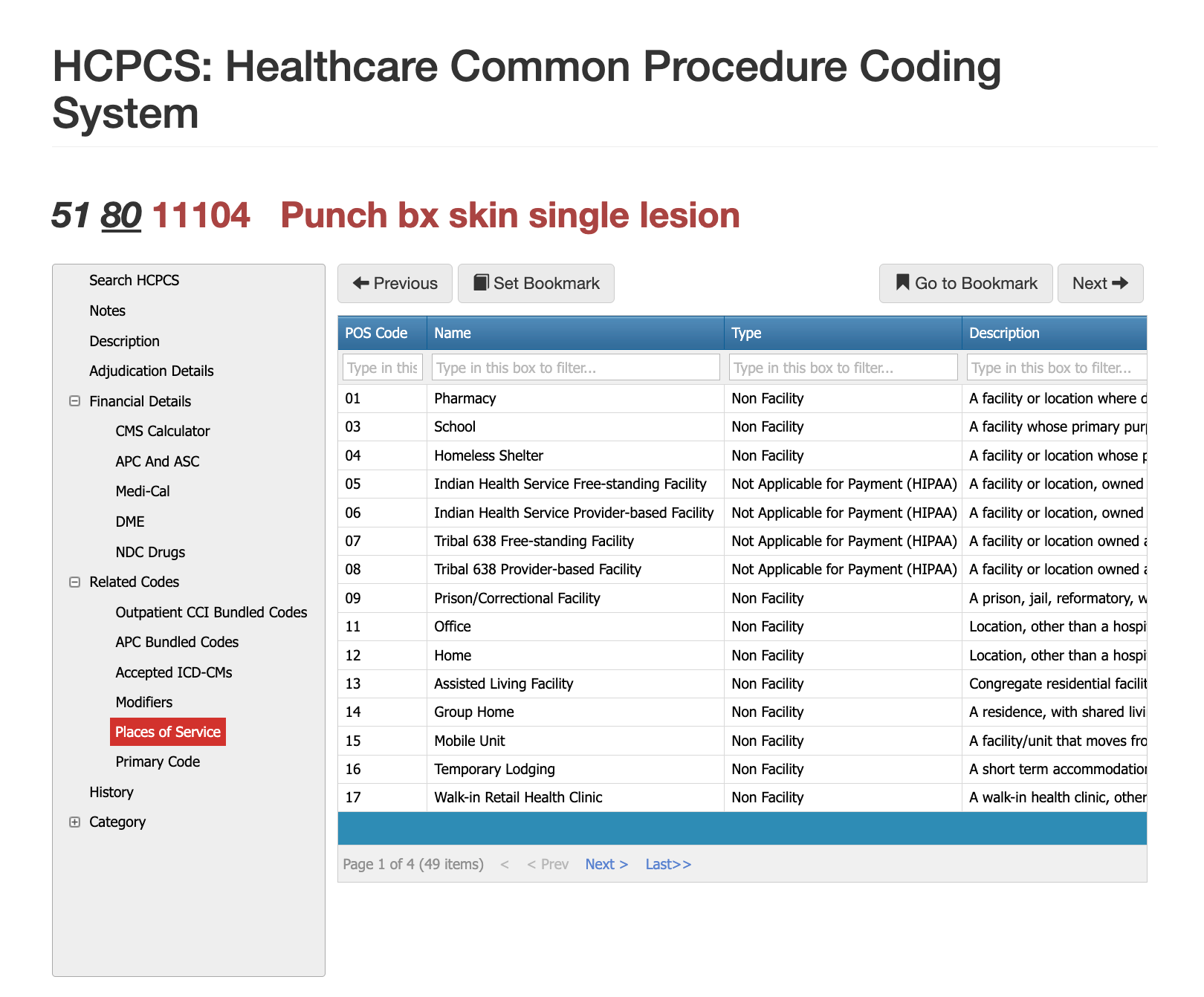
Places of Service for CPT Code 11104
CPT 11104 is most commonly billed in outpatient clinical settings such as physician offices, dermatology suites, and outpatient hospital departments. Ambulatory surgery centers may also report 11104 when performing biopsies on anatomically sensitive areas requiring specialized equipment. Claims reviewers ensure that the POS reflects a setting where biopsy instruments, sterile technique, and specimen handling procedures are properly supported. Billing 11104 in a non-clinical environment or inappropriate POS often results in an automatic denial.
Proper Documentation for CPT Code 11104
To support CPT 11104, documentation must clearly describe the lesion, the medical rationale for biopsy, the tangential technique used, and specifics such as anatomic location, specimen handling, and patient tolerance. The operative note should indicate that tissue was obtained for histopathology and sent to a lab. Providers should avoid vague statements such as “biopsied lesion” or “removed sample” without specifying technique, as payers may reclassify these as debridements or simple removals. Strong documentation includes the pre- and post-operative clinical impression and demonstrates why a tangential biopsy, rather than a punch or excisional procedure, was clinically appropriate.
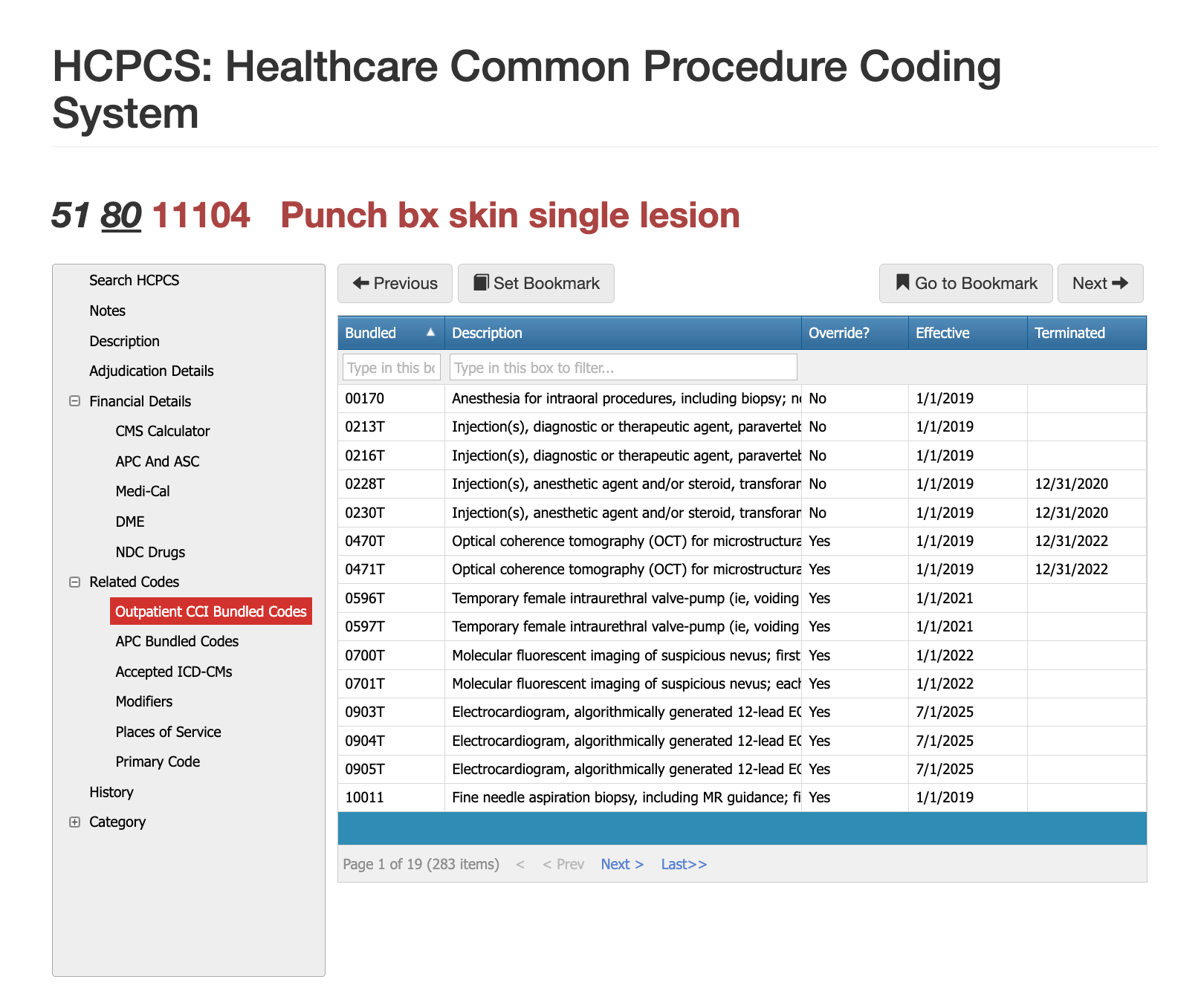
Related CPT Codes for 11104
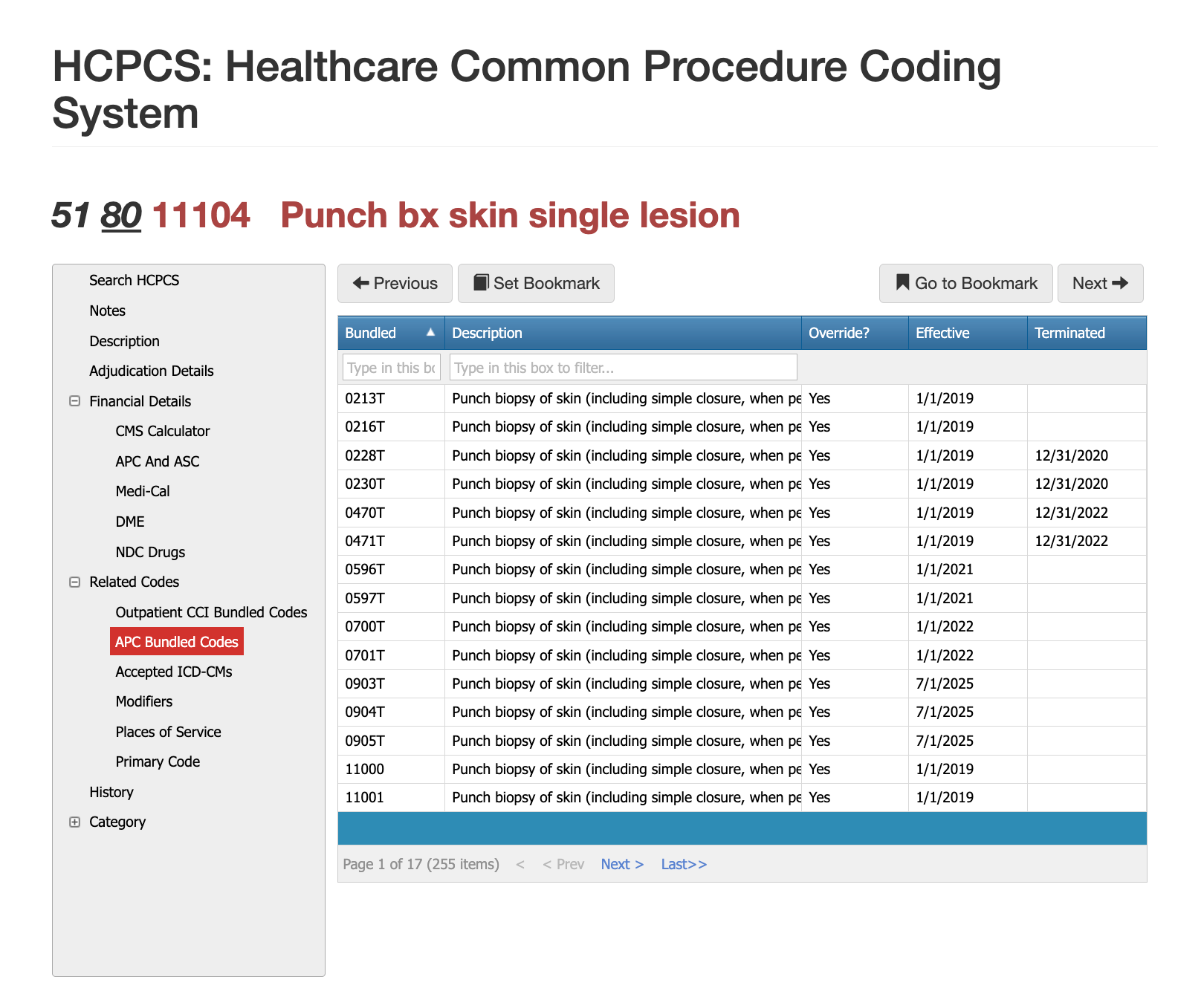
While 11102 was terminated, 1105, 11106, and 11107 are viable options based on the Add-on codes and whether it was a tangential biopsy or a punch biopsy. See the table below for more detailed information.
| Code | Description | How It Compares to 11104 |
|---|---|---|
| 11102 | Tangential biopsy, single lesion (older code) | 11104 is the updated, currently active code; 11102 is no longer used. |
| 11105 | Tangential biopsy, each additional lesion | Add-on code used with 11104. |
| 11106 | Punch biopsy of skin (single lesion) | Involves deeper sampling with a punch tool; not interchangeable. |
| 11107 | Punch biopsy, each additional lesion | Add-on code similar in function but for punch technique. |
When can you use Modifier 25 with 11104?
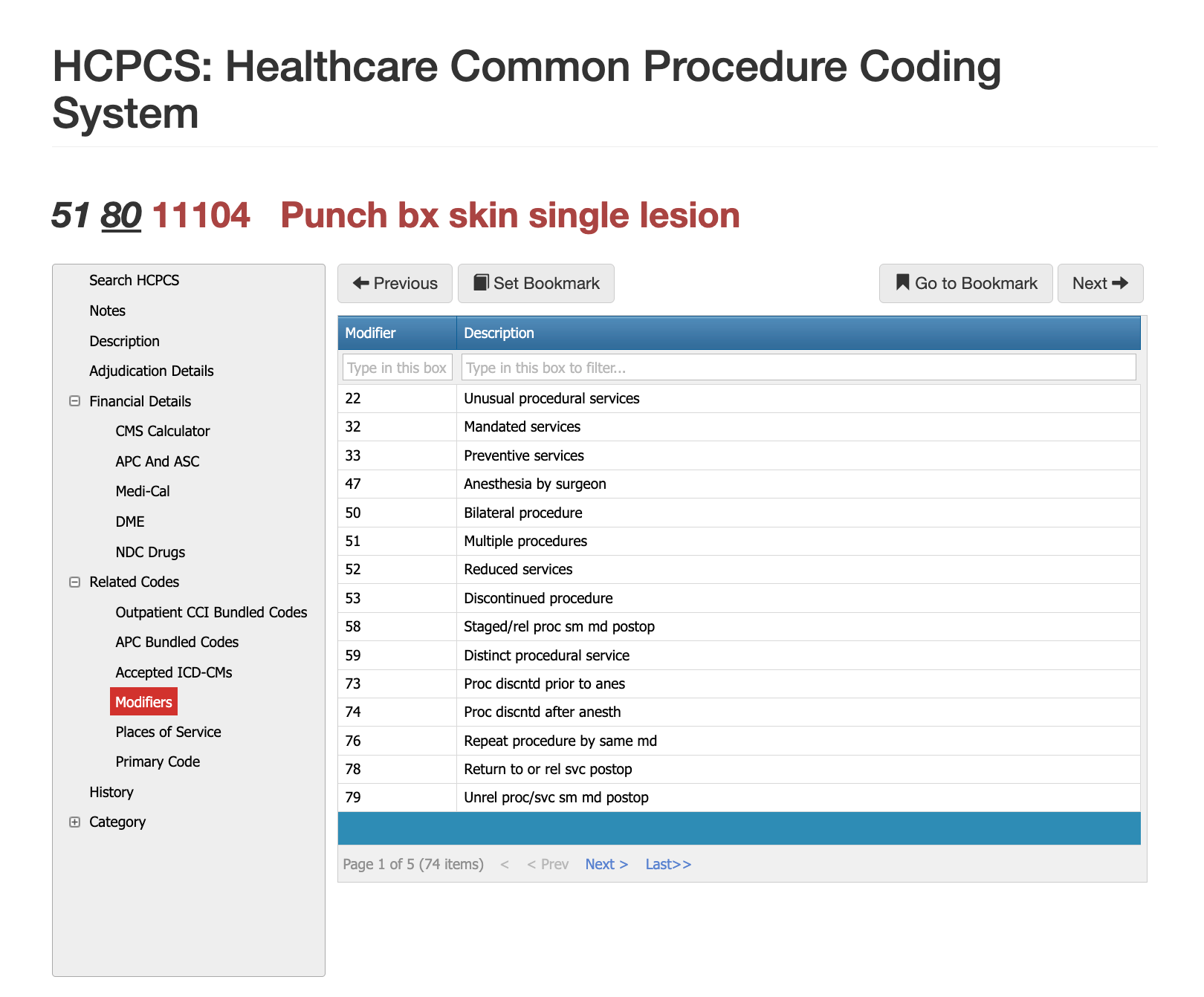
Modifier 25 is appended when a medically necessary evaluation and management service is performed on the same day as the biopsy. The E/M service must address problems beyond the decision to perform the biopsy. Claims examiners frequently deny modifier 25 when documentation fails to demonstrate separate clinical reasoning.
When can you use Modifier 59 with 11104?
Modifier 59 may be required when multiple procedures or biopsies occur across different anatomic sites or when payer systems bundle services under CCI edits. The documentation must clearly distinguish between procedural areas to justify its use.
When can you use Modifier RT/LT with 11104?
These modifiers apply when the biopsy occurs on the right or left side of the body. Laterality helps payers track repeat procedures and prevent duplicate denials.
Most Common Reasons for 11104 CPT Denials
The most frequent denials occur when documentation does not specify the tangential technique, fails to describe the lesion, or omits the clinical rationale for the biopsy. Payers may also deny claims when pathology results indicate no specimen was received or when the reported diagnosis reflects a cosmetic concern. Downcoding is common when the payer believes a simple lesion removal or shaving was performed rather than a diagnostic biopsy. Finally, claims are denied when providers bill 11104 for additional lesions but fail to append the appropriate add-on codes.
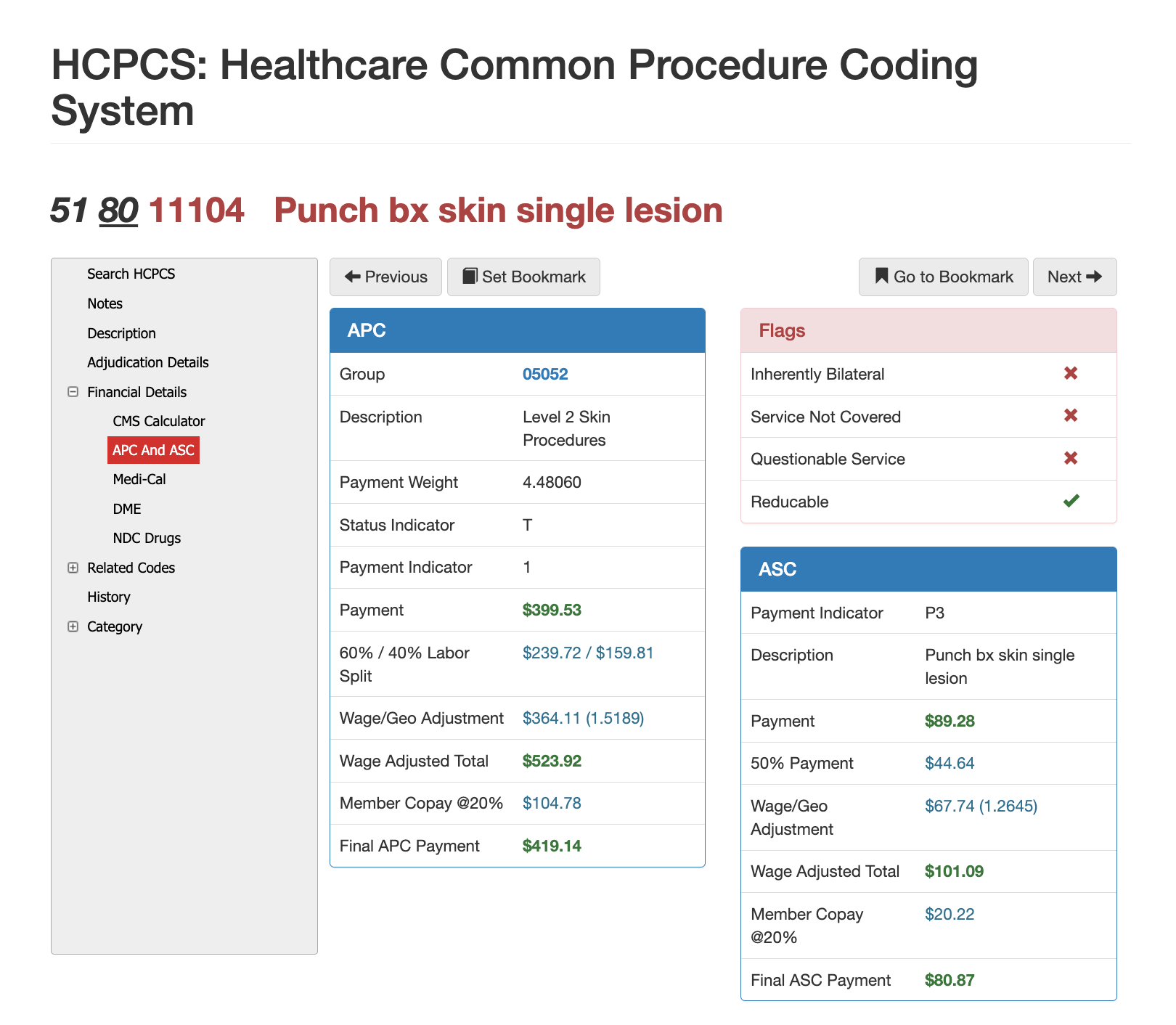
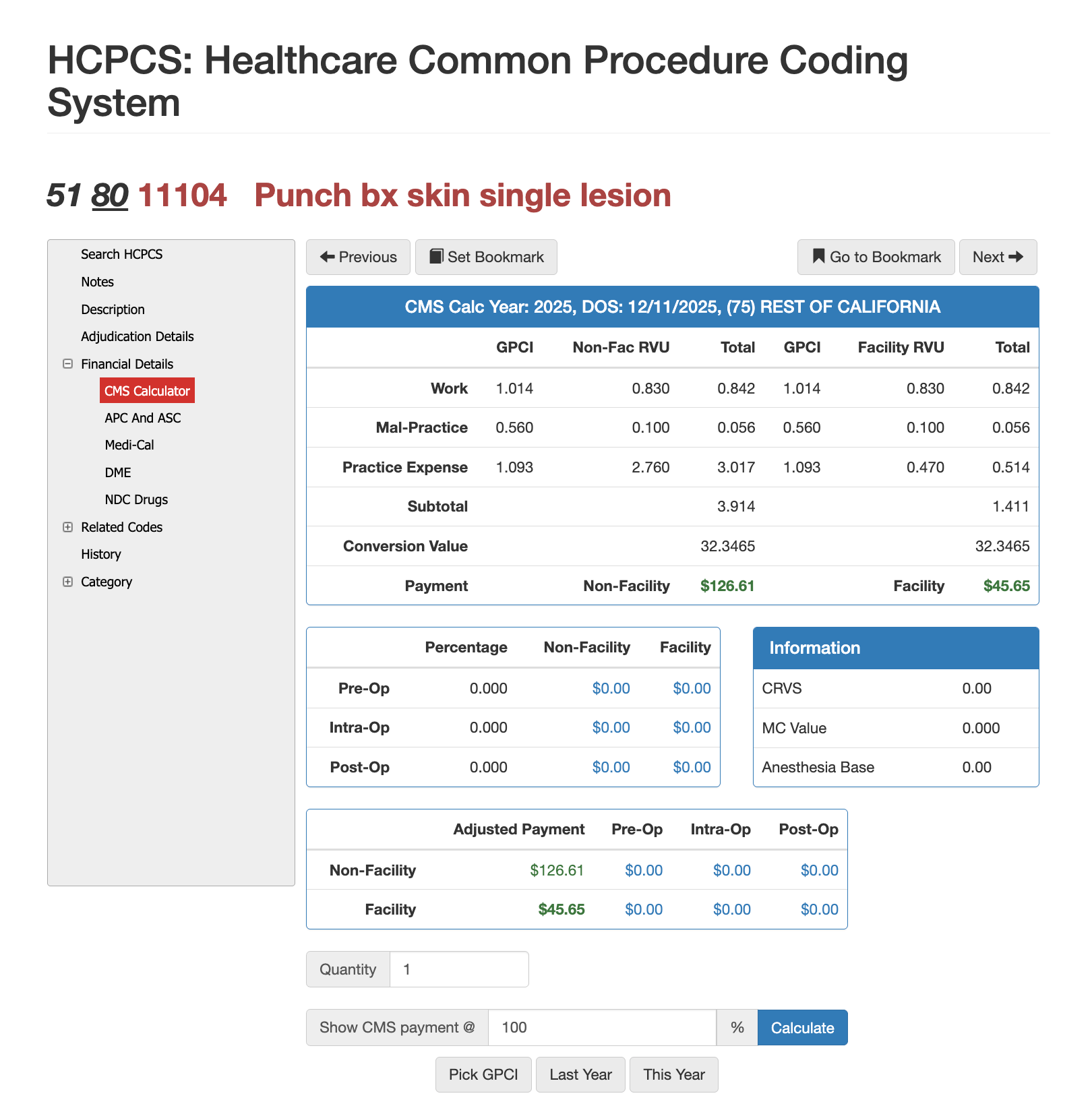
RVUs and Financials for CPT Code 11104
RVU Negotiation Guide for CPT 11104
Reimbursement for 11104 depends on national RVU assignments, geographic adjustments, and payer fee schedules. Because dermatologic procedures are often subject to minor surgical payment rules, payers may bundle certain services or require global period adherence. Using Virtual AuthTech for payers or iVECoder for providers allows users to model contract rates, compare facility versus office reimbursement, and evaluate whether current pricing aligns with CMS updates. These tools also help organizations detect inappropriate downcoding or overcoding of biopsy services, creating clearer financial expectations and improving audit readiness.
The Easier Way to Research codes
For more than 30 years, PCG Software has supported Health Plans, MSOs, IPAs, TPAs, and provider organizations in improving coding accuracy, strengthening compliance, and reducing fraud, waste, and abuse. Our solutions, including Virtual Examiner®, VEWS™, and iVECoder®, are built on decades of payer-side adjudication experience and reflect the same logic used by health plans nationwide. National regulatory guidance, payer policies, compliance standards, and large-scale claims review patterns inform this CPT 69210 analysis.
Toss out the CPT book.
Stop researching articles.
Sign up for iVECoder today!
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others