Crisis or Emergency scenarios for 88365
While CPT 88365 is not a “crisis” code, it is frequently used in
urgent diagnostic scenarios, such as rapid evaluation of suspected leukemias, lymphomas, congenital abnormalities, or high-risk oncologic conditions where immediate genetic clarification influences treatment decisions. In these cases, the CPT code remains 88365 for the initial probe, but documentation should reflect the
clinical urgency, the
specific diagnostic question, and the
reason rapid FISH testing was medically necessary. This helps prevent medical necessity denials, especially when expedited testing incurs higher cost or faster turnaround time requirements.
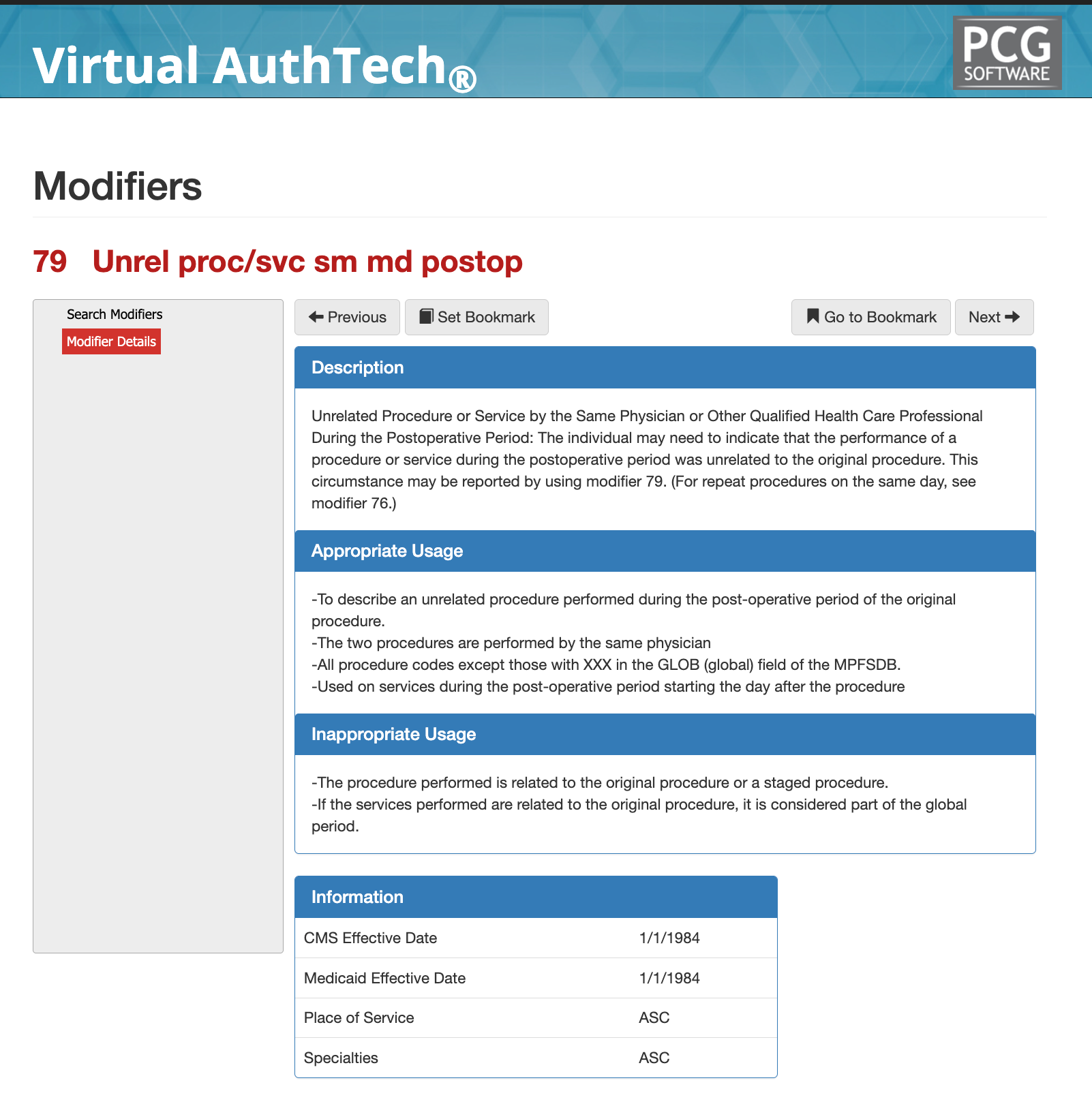
Modifier 79 - Guide on when, how, and what to use it for
Modifier 79 Quick Summary
Modifier 79 is used to report an unrelated procedure or service performed by the same physician or qualified health care professional during the postoperative (global) period of a prior procedure. Its purpose is to clearly communicate to the payer that the new service is not part of the original surgery’s global package and should therefore be reimbursed separately. From a payer and CMS perspective, Modifier 79 is a global-period override modifier, not a bundling or payment sequencing modifier. When applied correctly, it resets the global period for the new procedure and allows payment outside the original postoperative care window.
Modifier 79 Description & Usage
Modifier 79 indicates that the performance of a procedure or service during the postoperative period was unrelated to the original procedure. This modifier is used when the same physician performs the unrelated service after the original surgery, beginning the day after the initial procedure. It applies to procedures with assigned global periods and is reported on services that are clinically independent of the original surgical treatment.
When can I use Modifier 79 appropriately?
Modifier 79 should be used when all of the following conditions are met:
- A procedure is performed during the postoperative (global) period of a prior procedure
- The new procedure is unrelated to the original surgery
- The service is performed by the same physician or qualified health care professional
- The service is not staged, planned, or related to the original procedure
- The service begins after the day of surgery (not on the same day)
Typical scenarios include treatment of a new condition, injury, or diagnosis that arises independently during the global period of a previous procedure. From a claims adjudication standpoint, Modifier 79 tells the payer that the global surgical package does not apply to the subsequent service and that a new global period may begin based on the second procedure’s global assignment.
Modifier 79 and Global Surgical Periods
Modifier 79 overrides the original procedure’s global period and establishes a new global period for the unrelated procedure being reported. This is a key distinction from other postoperative modifiers.CMS evaluates global periods based on the Medicare Physician Fee Schedule global indicator. Modifier 79 may be used on procedures with assigned global days, except those marked with XXX global indicators, which do not have postoperative periods. Claims reviewers expect documentation to clearly demonstrate that the diagnosis, clinical intent, and operative site are independent of the original surgery.
When is it not appropriate to use Modifier 79?
Modifier 79 should not be reported in the following situations:
- The procedure is related to the original surgery
- The service represents postoperative care, complications, or follow-up treatment
- The procedure was planned or staged at the time of the original surgery
- The service occurs on the same day as the original procedure
- The procedure is part of the original procedure’s global package
If the subsequent service is related, staged, or planned, other modifiers—such as Modifier 58 or Modifier 78—may apply instead. Using Modifier 79 to bypass the global period for related care is a frequent cause of denials and audit findings.
Example 1: Related Postoperative Care or Complication
A patient undergoes a laparoscopic cholecystectomy and returns during the global period with postoperative bile leakage requiring surgical intervention. Although a new procedure is performed, the operative note confirms the condition is a complication of the original surgery. Because the service is directly related to postoperative management, Modifier 79 is inappropriate. Depending on the circumstances, Modifier 78 may apply, but the service cannot be reported as unrelated.
Example 2: Planned or Staged Procedure Identified at Initial Surgery
During an initial colorectal surgery, the surgeon documents a planned second-stage procedure to be performed during the global period once healing occurs. When the follow-up procedure is later performed, it cannot be reported with Modifier 79, as the service was anticipated and part of the original treatment plan. In this scenario, Modifier 58—not Modifier 79—would be the appropriate modifier if separate payment is warranted.
Example 3: Service Included in the Global Surgical Package
A patient returns for suture removal, wound checks, or routine postoperative evaluations following a surgical procedure. Even if additional minor interventions are performed, the documentation shows these services fall within expected postoperative care. Reporting Modifier 79 in this case is inappropriate because the services are inherently included in the original procedure’s global package and do not represent a separate, unrelated surgical event.
Documentation Requirements for Modifier 79
Strong documentation is critical for Modifier 79 compliance. The medical record should clearly establish:
- A new or separate diagnosis
- Clinical findings unrelated to the original surgery
- Distinct operative notes or procedural documentation
- Clear separation from postoperative follow-up care
- A rationale explaining why the service is not part of the original treatment plan
Vague statements such as “unrelated” without a clinical explanation are insufficient and frequently flagged during audits.
Example 1: New Diagnosis During the Global Period
A patient undergoes arthroscopic knee surgery and later presents during the postoperative period with acute abdominal pain. Evaluation confirms appendicitis, requiring an urgent appendectomy performed by the same surgeon. The operative note clearly documents a new diagnosis unrelated to the musculoskeletal system, distinct clinical findings, and a separate surgical plan. The record establishes that the appendectomy is not connected to the prior orthopedic procedure, supporting appropriate use of Modifier 79.
Example 2: Separate Anatomical Site and Clinical Condition
Following a dermatologic excision of a malignant lesion on the left forearm, the patient returns during the global period for surgical management of a symptomatic lipoma on the upper back. Documentation specifies a different anatomical site, unrelated pathology, and a distinct operative report. The surgeon explicitly notes that the second procedure addresses a separate condition with no clinical relationship to the original excision, meeting Modifier 79 requirements.
Example 3: Unrelated Surgical Event With Independent Treatment Plan
A patient undergoes cataract extraction and subsequently presents within the global period with an incarcerated inguinal hernia requiring surgical repair. The medical record includes a new diagnosis, separate preoperative assessment, and an operative note outlining an independent treatment plan. The documentation makes clear that the hernia repair is unrelated to postoperative ophthalmologic care and is not a complication or continuation of the original surgery, supporting compliant use of Modifier 79.
Helpful tips on Modifier 79
Modifier 79 vs Modifier 58 vs Modifier 78
Modifier 79 is commonly confused with Modifiers 58 and 78 because all three involve procedures performed during a global period. However, their purposes are fundamentally different. Modifier 79 applies
only to unrelated procedures. Modifier 58 applies to
staged or planned procedures related to the original surgery. Modifier 78 applies to
unplanned returns to the operating room for complications associated with the initial procedure. Payers evaluate these modifiers differently, and incorrect selection can lead to payment reductions, claim reprocessing, or recoupments.
Common Modifier 79 Denials Triggers and Payer Logic
Modifier 79 is frequently denied or flagged for audit because it directly affects global surgical payment rules. Claims are commonly challenged when the diagnosis appears clinically related to the original procedure, the operative or anatomical site overlaps without a clear explanation, or the documentation resembles routine postoperative care rather than a truly separate surgical event. Additional risk indicators include repeated use of Modifier 79 for the same patient and provider, or patterns suggesting the modifier is being applied to bypass global period restrictions rather than to report a legitimately unrelated service.
From a payer adjudication perspective, Modifier 79 functions as a global period override signal. When accepted, it instructs the claims system to treat the service as a separate and unrelated procedure, restarting payment logic rather than bundling it into postoperative care. However, approval is driven by documentation—not the modifier itself. Payers and CMS contractors evaluate diagnosis codes, timing, operative reports, anatomical detail, and prior claim history to validate that the procedure is truly unrelated. Without clear, defensible documentation supporting clinical independence, Modifier 79 is unlikely to survive automated edits or manual review.
Compliance Considerations for Modifier 79
Modifier 79 is appropriate when used correctly but represents a high-risk modifier from a compliance perspective. Overuse or misuse may indicate attempts to circumvent global surgical rules. Best practices include:
- Using Modifier 79 sparingly and intentionally
- Ensuring diagnoses clearly differ from the original procedure
- Maintaining detailed operative and clinical documentation
- Avoiding Modifier 79 when follow-up care could reasonably be expected
Health plans and CMS auditors often view inappropriate Modifier 79 usage as a signal for broader coding pattern review.
Summary on Modifier 79
Modifier 79 is designed to allow reimbursement for
truly unrelated procedures performed during a postoperative period, not to bypass global surgical rules. When used correctly, it supports accurate claims processing and fair reimbursement. When used incorrectly, it is among the most common triggers of denials, audits, and payment recoveries. Understanding the distinction between unrelated care and postoperative or staged services is essential to compliant Modifier 79 reporting and long-term revenue protection.
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others