CPT 99214 - Established Patient Consult for 30-39 Minutes in Outpatient Setting
What will this article teach you about 99214
CPT Code 99214 represents an established patient office or outpatient visit requiring
moderate medical decision-making (MDM) or
30–39 minutes of total time spent on the date of the encounter. It is one of the most commonly billed E/M codes because it reflects visits where the provider evaluates multiple conditions, adjusts treatment plans, interprets tests, or manages moderate risks. In this guide, we clarify AMA and CMS requirements, documentation elements, payer expectations, and common denial reasons—plus financial implications that coders, auditors, and compliance teams must understand. This article mirrors exactly how claims examiners evaluate 99214 so you can submit or review claims with full confidence.
The Who, What, When for billing and paying for CPT Code 99214
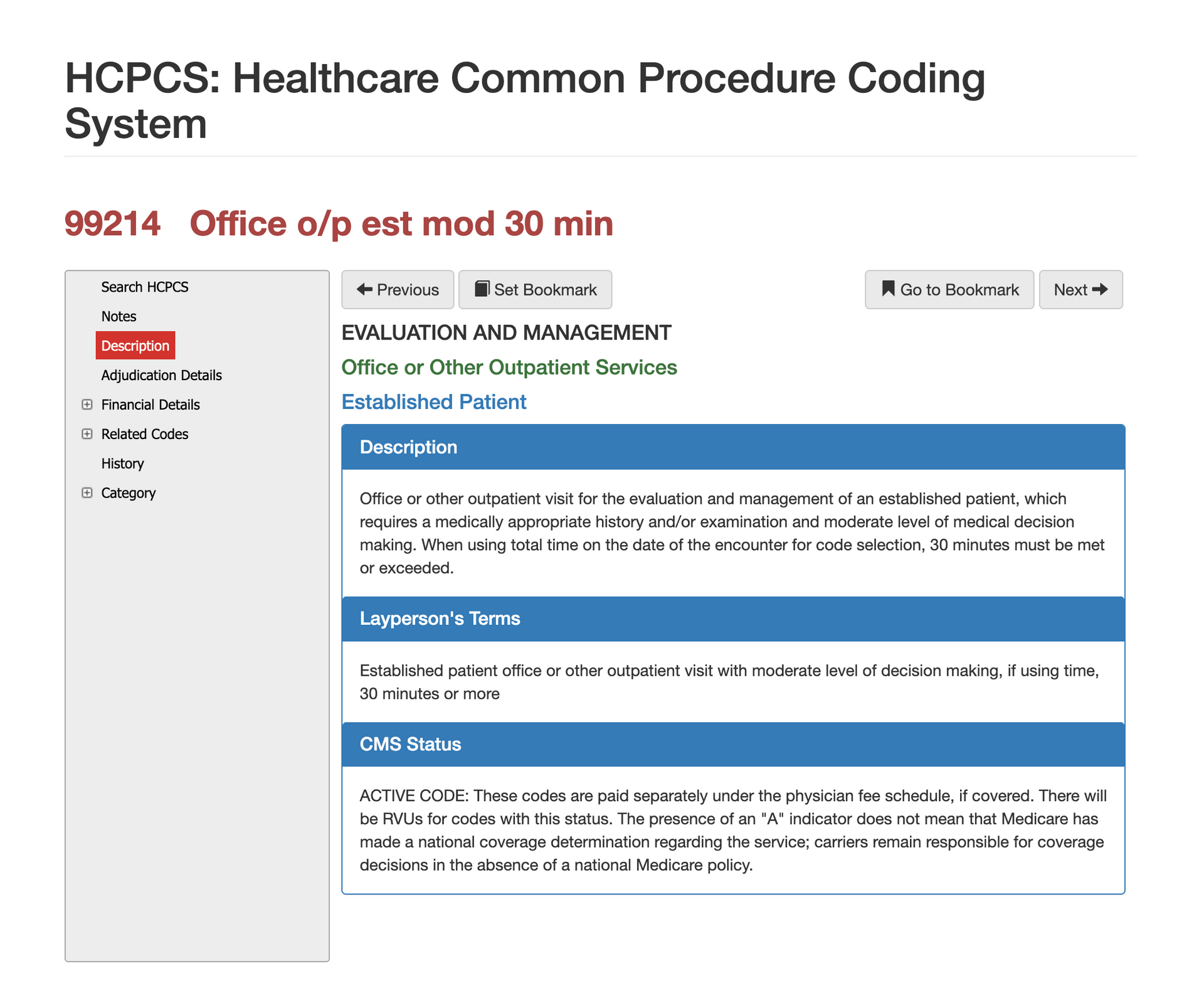
AMA Definition of CPT Code 99214:
Office or outpatient visit for the evaluation and management of an established patient requiring a medically appropriate history and/or exam and moderate level of medical decision-making OR 30–39 minutes of total time on the date of the encounter.
Layperson Description for CPT Code 99214:
99214 is used when a patient returns with multiple concerns or a condition serious enough to require deeper assessment, medication management, or treatment changes. These visits involve more thinking, more risk, and more decision-making than a simple check-up.
When is CPT Code 99214 Used?
CPT 99214 should be used when the provider’s work meets moderate MDM OR when the total time on the date of service is 30–39 minutes. To qualify for moderate medical decision-making, the visit typically includes reviewing multiple data sources, managing chronic conditions that require ongoing adjustment, or addressing new problems with potential complications. Examples include medication titration, interpreting test results, coordinating specialty care, or managing chronic disease exacerbations.
99214 does not require a comprehensive exam or detailed HPI under 2021 E/M rules—only medically appropriate documentation and evidence of moderate complexity or time.
Who bills for CPT Code 99214?
Primary care physicians, internists, pediatricians, family medicine providers, and specialists across nearly all outpatient disciplines frequently bill 99214. Nurse practitioners and physician assistants also use this code when their documentation satisfies the criteria and payer policies allow it. Mental health clinicians may bill 99214 when performing E/M services involving medication management. Across all specialties, claims auditors look closely at whether the note supports moderate complexity rather than low complexity (99213).
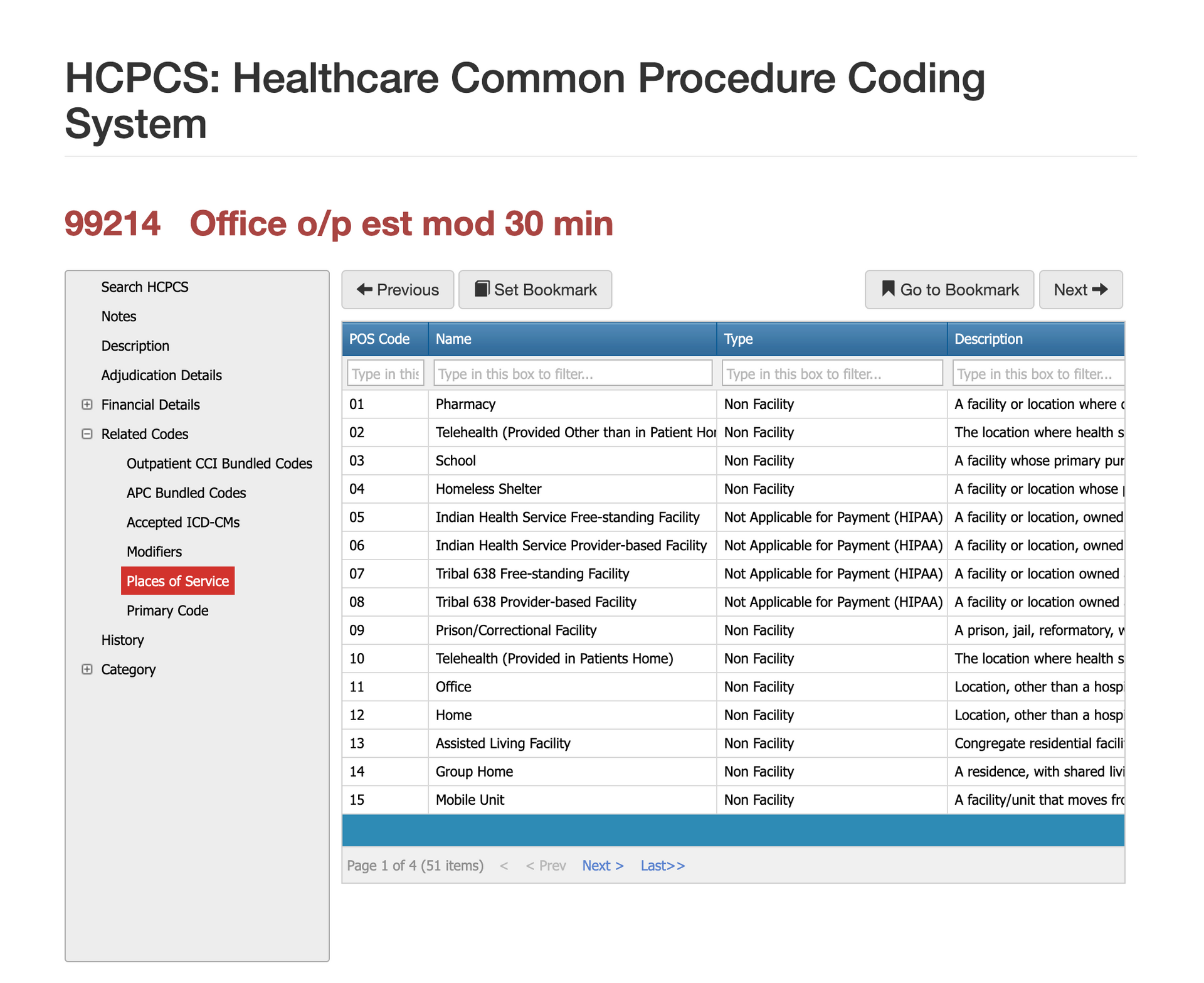
Places of Service for CPT Code 99214
The most common POS codes for 99214 include:
- 11 – Office (most frequent)
- 22 – Hospital outpatient
- 19 – Off-campus outpatient hospital
- 02 or 10 – Telehealth
Payers verify that the POS aligns with the documentation and that telehealth services follow federal and commercial coverage rules for 99214.
Diagnosis and ICD-10 for CPT Code 99214
Diagnosis codes must support
moderate complexity or use of time, such as chronic illness with exacerbation, multiple chronic conditions, cognitive disorders requiring medication adjustments, or diagnostic uncertainty. Vague or nonspecific diagnoses often result in downcoding to 99213. Strong ICD-10 documentation increases the likelihood that the service will be accepted at the moderate level.
Proper Documentation for CPT Code 99214
To justify billing 99214, documentation must demonstrate one of the following:
MDM Requirements (Moderate Complexity)
Moderate MDM requires meeting two of three elements:
- Problem Complexity: One or more chronic illnesses with exacerbation/progression, OR two or more stable chronic conditions, OR a new problem with uncertain prognosis.
- Data Review: Reviewing external notes, test results, ordering tests, or independent interpretation of prior studies.
- Risk: Moderate risk of morbidity from treatment decisions, diagnostic testing, or medication management (e.g., controlled substances, new prescription initiation, dosage changes).
OR Time Requirement
Total time on the date of visit = 30–39 minutes, including:
- Reviewing prior notes
- Examining the patient
- Ordering or reviewing tests
- Documenting in the chart
- Coordinating care or communicating with other providers
- Important:
Time
does not include staff tasks, non-medical discussions, or time spent outside the date of service.
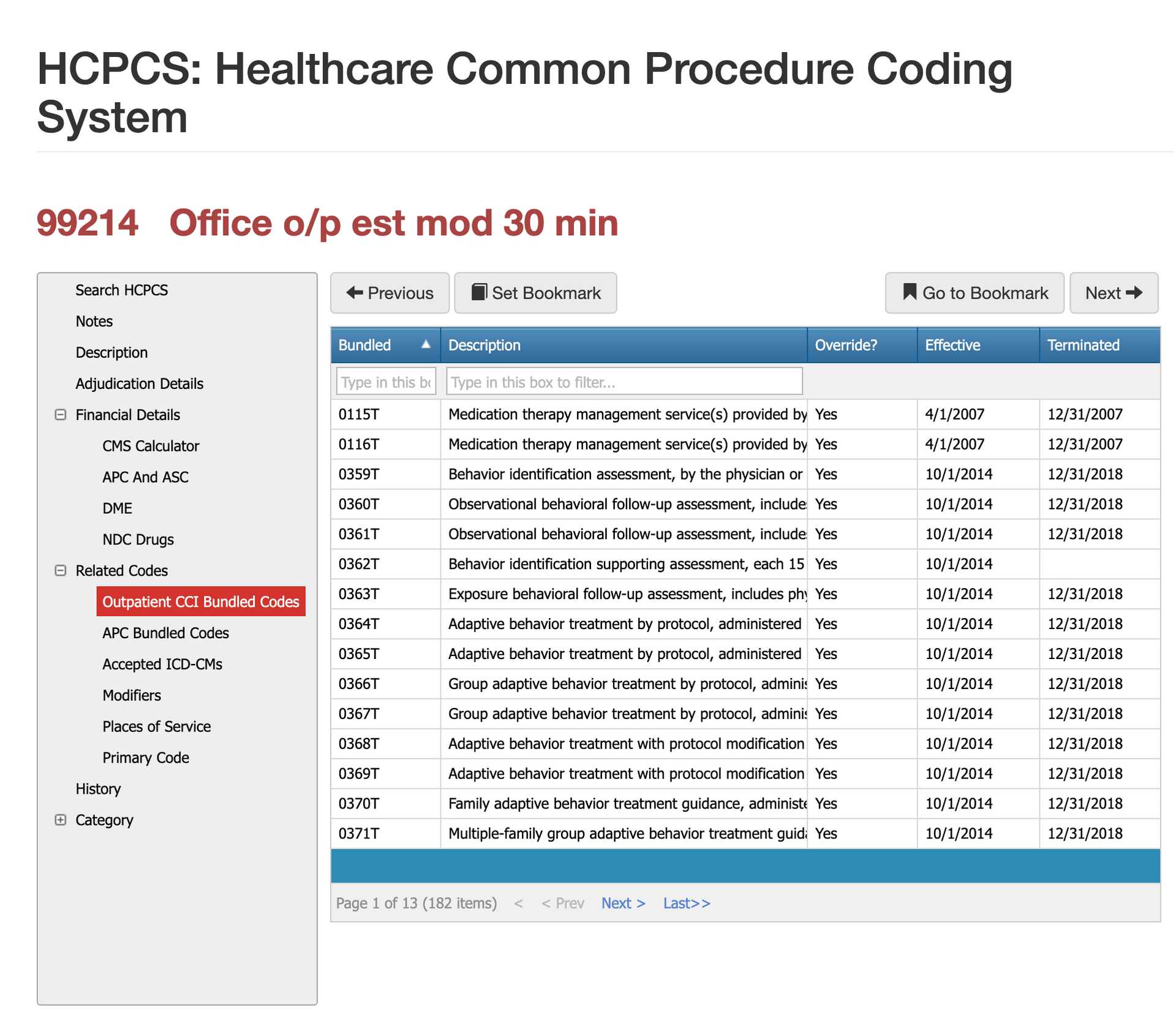
Bundled Codes for CPT Code 99214
CPT 99214 interacts with multiple CCI edits because E/M services are often bundled into procedural encounters unless modifier 25 or 24 is applied. In outpatient hospital settings, 99214 is reimbursed under the outpatient E/M APC groups, but separate payment may depend on payer policy. ASCs typically bundle E/M visits into the procedure unless the service is unrelated and clearly documented.
Virtual Examiner and
iVECoder can help detect bundling conflicts by comparing billed codes, modifiers, and clinical notes before submission, preventing incorrect unbundling and financial loss.
Related CPT Codes for 99214
CPT 99214 belongs to the evaluation and management family of outpatient visit codes. Understanding how it differs from surrounding codes—especially 99213 and 99215—helps providers and payers choose the correct level based on MDM or time.
| Code | Description | MDM Level | Time Requirement | Key Difference |
|---|---|---|---|---|
| 99212 | Established patient visit | Straightforward | 10–19 min | Very limited problems; low complexity |
| 99213 | Established patient visit | Low MDM | 20–29 min | Routine, stable conditions; minimal risk |
| 99214 | Established patient visit | Moderate MDM | 30–39 min | Multiple conditions, medication changes, test interpretation |
| 99215 | Established patient visit | High MDM | 40–54 min | Severe issues, significant data review, high-risk decisions |
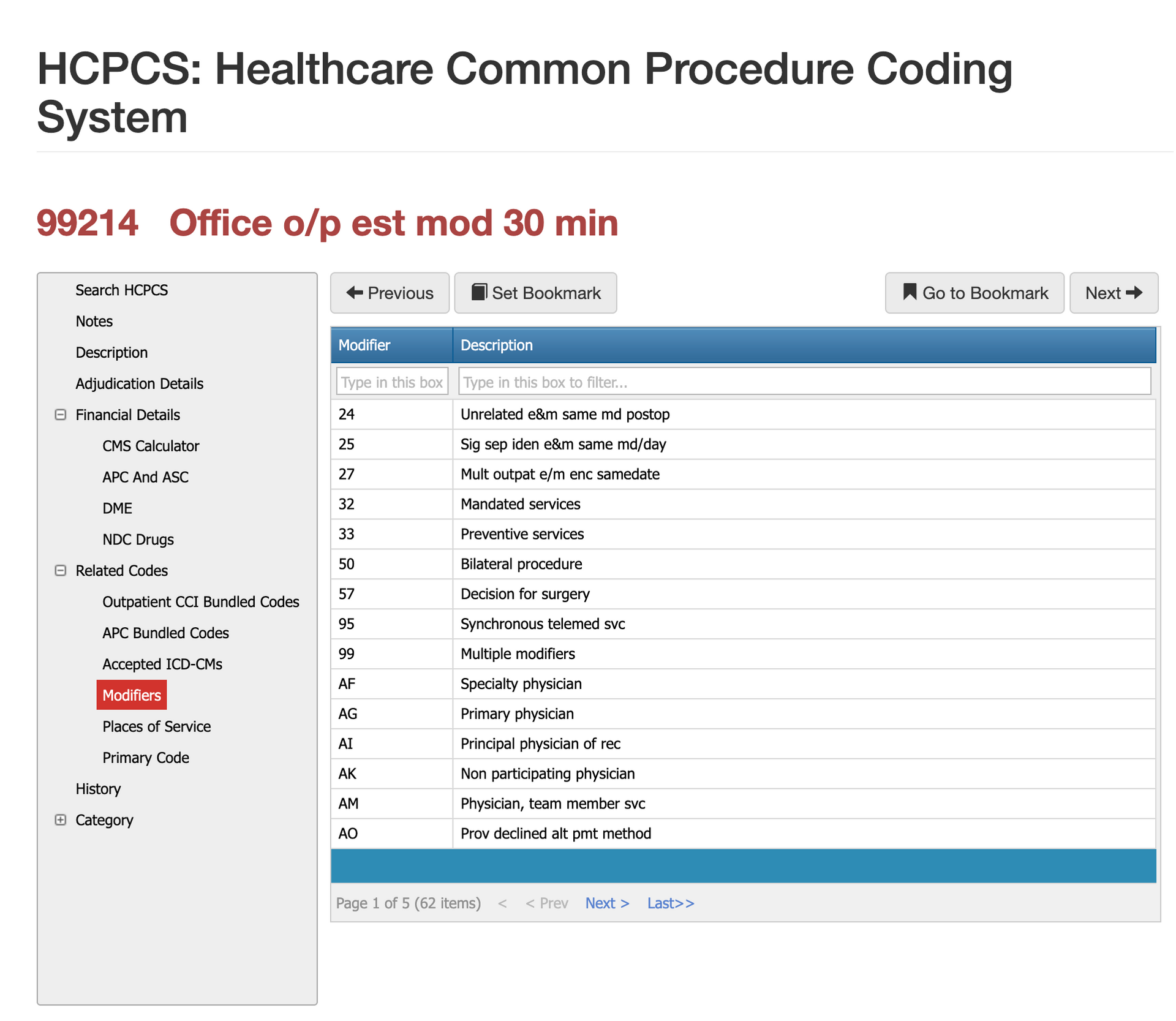
Modifier Guidance for CPT Code 01996
Only a few modifiers commonly pair with 99214, and each requires strict documentation.
Modifier 25 for CPT Code 99214
Used when a procedure is performed on the same day and the E/M visit involved additional, medically necessary work beyond the procedure.
Modifier 24 for CPT Code 99214
Applied when a patient is in a global surgical period but the visit addresses a completely different problem.
Modifier 52 or 53 for CPT Code 99214
Rarely used but applicable in unusual circumstances where the service was limited.
Incorrect modifier use is a top source of audit findings for E/M codes.
Most Common Reasons for 99214 CPT Denials
The top reasons 99214 gets denied include:
- MDM not meeting moderate complexity (most common)
- Insufficient documentation or lack of decision-making detail
- Downcoding to 99213 due to vague narratives (“follow-up visit, stable”)
- Incorrect use of modifier 25 on procedure days
- Diagnosis not supporting complexity
Auditors focus heavily on whether the note shows active management—not passive follow-up.
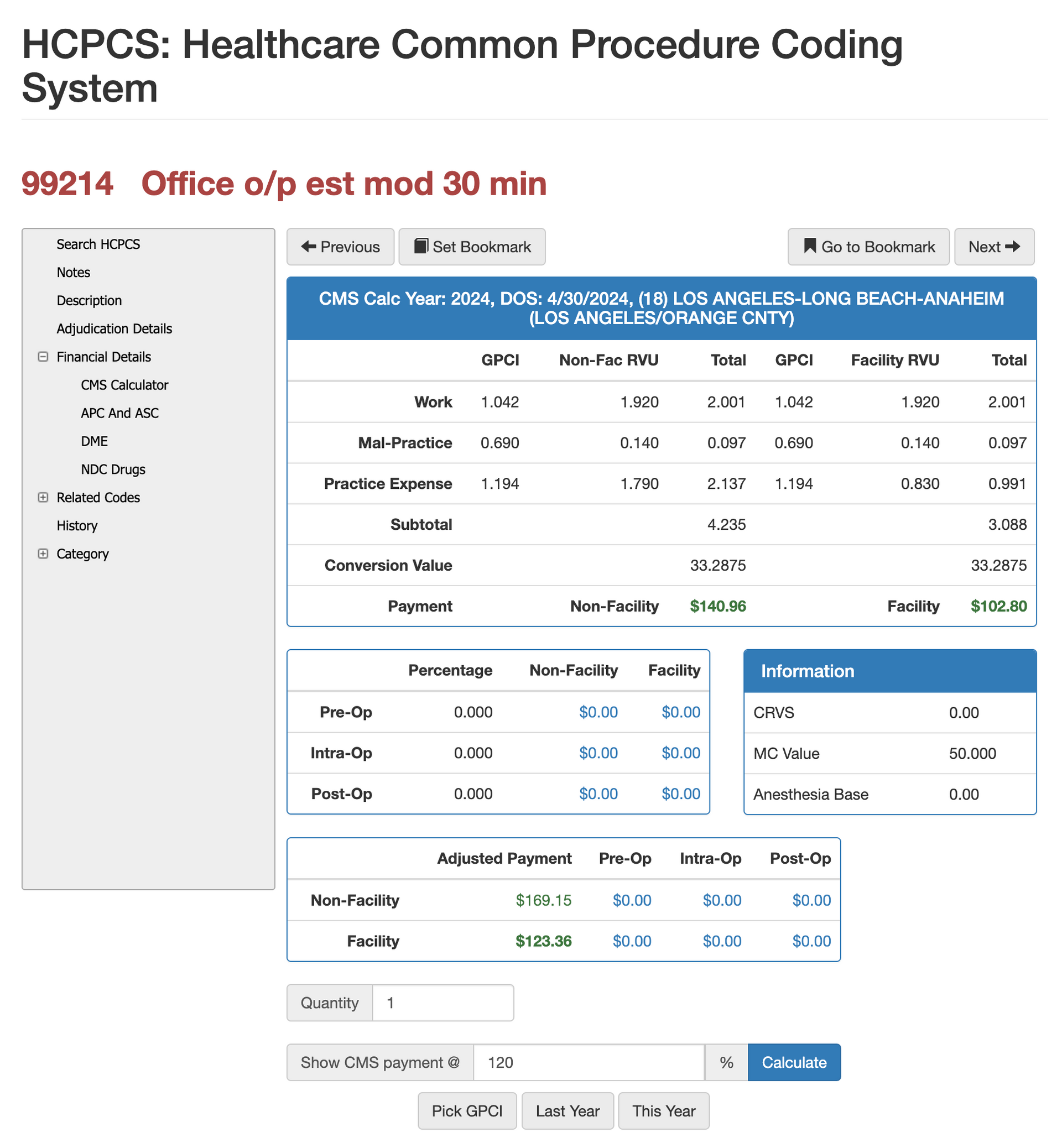
RVUs and Financials for CPT Code 99214
How to look at and negotiate RVUs for 99214
Because CPT 99214 carries one of the highest work RVUs among established-patient E/M visits, it often becomes a focal point during payer–provider contract negotiations. Its reimbursement varies by geographic region (GPCI), facility vs. non-facility status, and the percentage of Medicare that a payer uses as its benchmark. Practices frequently evaluate the RVU value of 99214 when determining whether commercial contracts fairly compensate for the moderate-complexity decision-making typically required during chronic disease management, medication adjustments, and ongoing patient monitoring.
Tools such as
Virtual AuthTech and
iVECoder allow payers and providers to model 99214 reimbursement across multiple Medicare percentages, compare payment variations by state, and analyze how RVU adjustments affect overall profitability. These simulations provide a data-driven foundation for negotiating fair rates, identifying underperforming contracts, and ensuring alignment with CMS fee schedule updates—all while maintaining compliance and financial integrity.
The Easier Way to Research codes
For more than 30 years, PCG Software has supported Health Plans, MSOs, IPAs, TPAs, and provider organizations in improving coding accuracy, strengthening compliance, and reducing fraud, waste, and abuse. Our solutions, including Virtual Examiner®, VEWS™, and iVECoder®, are built on decades of payer-side adjudication experience and reflect the same logic used by health plans nationwide. National regulatory guidance, payer policies, compliance standards, and large-scale claims review patterns inform this CPT 69210 analysis.
Toss out the CPT book.
Stop researching articles.
Sign up for iVECoder today!
Subscribe
Only get notifications when a new article has been published
Contact Us
We will get back to you as soon as possible.
Please try again later.
Free Payer Claims Audit
Complete the form, and we'll contact you to schedule an introductory meeting and discuss our FREE 3-year claims audit to identify areas for cost containment and compliance.
Contact Us
We will get back to you as soon as possible.
Please try again later.
About PCG
For over 30 years, PCG Software Inc. has been a leader in AI-powered medical coding solutions, helping Health Plans, MSOs, IPAs, TPAs, and Health Systems save millions annually by reducing costs, fraud, waste, abuse, and improving claims and compliance department efficiencies. Our innovative software solutions include Virtual Examiner® for Payers, VEWS™ for Payers and Billing Software integrations, and iVECoder® for clinics.
Click to share with others